What it is
→ Vascular occlusion protocol refers to the structured emergency management plan followed when dermal filler injections accidentally block a blood vessel.
→ Vascular occlusion occurs when filler material obstructs arterial or venous blood flow, leading to skin blanching, severe pain, and potential tissue necrosis.
→ Though rare, it is considered one of the most serious complications of injectable aesthetic procedures.
→ A vascular occlusion protocol ensures rapid recognition, immediate intervention, and proper follow-up, preventing permanent damage such as skin loss, scarring, or blindness (if near the eyes).
Why it’s done
→ The protocol is performed to:
- Save tissue by restoring blood circulation quickly.
- Prevent necrosis (death of skin tissue).
- Avoid permanent scarring or deformities.
- Protect vision in cases where occlusion occurs near the eye region.
- Provide patient safety and reassurance in cosmetic procedures.
→ Without a clear protocol, delays in treatment can result in severe medical and cosmetic consequences.
Alternatives
→ There is no true alternative to vascular occlusion protocol when an occlusion occurs. It is a medical emergency that requires immediate professional intervention.
→ Preventive strategies include:
- Using cannulas instead of sharp needles in high-risk zones.
- Injecting slowly with minimal pressure.
- Aspirating before injection to check for intravascular placement.
- Knowledge of vascular anatomy to avoid risky areas.
→ However, once occlusion happens, the only option is to follow the emergency protocol immediately.
Preparation
→ Clinics must be prepared with:
- Emergency kits containing high-dose hyaluronidase (for dissolving HA fillers).
- Sterile saline for flushing.
- Aspirin tablets to reduce clot formation.
- Topical nitroglycerin paste to dilate blood vessels.
- Warm compresses to increase circulation.
- LED or hyperbaric oxygen therapy access for severe cases.
- Emergency referral contacts (ophthalmology, hospital care).
→ Practitioners and staff should be trained regularly to recognize early signs and act immediately.
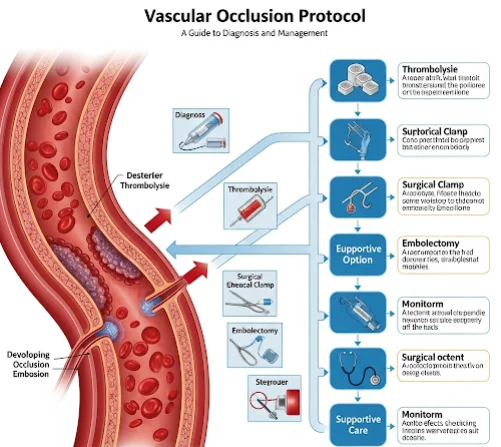
How it’s Done
→ A vascular occlusion protocol involves step-by-step intervention:
- Immediate recognition
- Look for sudden pain, blanching of the skin, dusky discoloration, or mottling.
- Stop injection immediately
- Do not continue injecting filler in the area.
- Massage and heat
- Apply warm compresses and massage the area to improve blood flow.
- Hyaluronidase injection
- Administer high-dose hyaluronidase (150–300 units or more, depending on severity) directly into and around the affected area.
- Repeat every 30–60 minutes as needed until reperfusion occurs.
- Adjunctive measures
- Apply nitroglycerin paste to dilate vessels.
- Give aspirin (oral, usually 300–325 mg) to reduce platelet aggregation.
- Consider low molecular weight heparin in severe cases (under physician guidance).
- Supportive therapy
- Oxygen supplementation.
- Hyperbaric oxygen therapy if available, for stubborn or severe cases.
- Antibiotics if tissue necrosis develops.
- Ophthalmic emergency (if vision is affected)
- Immediate referral to an ophthalmologist for intra-arterial hyaluronidase, retrobulbar injections, or advanced care.
- Follow-up
- Daily monitoring for skin healing.
- Scar management, if needed, with laser, microneedling, or PRP.
→ The first 90 minutes are critical; rapid action can mean the difference between full recovery and permanent damage.
Recovery
→ Recovery depends on the severity of the occlusion and how fast treatment was initiated:
- Early intervention → most patients recover fully within days to weeks.
- Delayed intervention → may result in partial necrosis requiring wound care, scar prevention, or reconstructive procedures.
- Ocular occlusions → prognosis varies; immediate ophthalmologic care is vital to preserve vision.
→ Long-term recovery may include:
- Scar management → silicone sheets, steroid injections, or laser therapy.
- Pigmentation correction → if skin discoloration remains.
- Psychological support → reassurance and counseling for patients after complications.
Complications
→ Even with prompt care, possible complications include:
- Skin necrosis → if circulation is not restored quickly.
- Scarring or fibrosis.
- Pigment changes (post-inflammatory hyperpigmentation or hypopigmentation).
- Chronic pain or sensitivity in the affected area.
- Vision loss if occlusion affects the retinal artery and is not treated immediately.
→ These risks highlight why vascular occlusion protocols must be standardized in all injection clinics.
Treatment options in Korea
→ Korea is globally recognized for aesthetic injection safety protocols, including advanced vascular occlusion management.
- Emergency readiness → top clinics always stock hyaluronidase, aspirin, nitroglycerin, and sterile kits for rapid response.
- Highly trained injectors → Korean dermatologists and plastic surgeons receive rigorous training in complication management.
- Advanced monitoring → AI-assisted imaging and dermoscopy are sometimes used to track skin reperfusion after occlusion.
- Collaboration with hospitals → strong referral systems to ophthalmology and emergency care for vision-related occlusions.
- Post-recovery programs → clinics provide scar prevention counseling, wound care, and aesthetic correction if needed.
- Medical tourism services → international patients are reassured by Korea’s strong safety culture and emergency preparedness.
→ With Korea’s emphasis on precision, safety training, and comprehensive aftercare, vascular occlusion protocols are considered among the most advanced in the world.