What it is
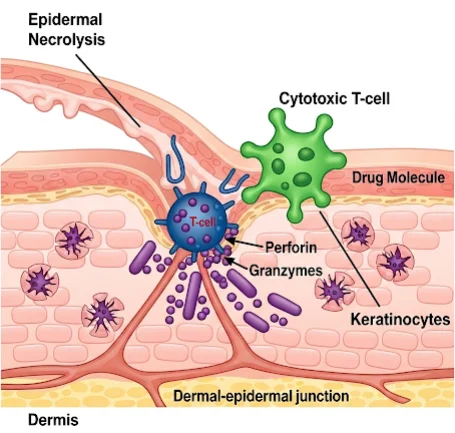
➝ Toxic epidermal necrolysis (TEN) is the most severe form of drug-induced mucocutaneous reaction, defined by >30% body surface area (BSA) detachment with mucosal involvement.
➝ It is considered a dermatologic emergency with mortality rates of 25–35%.
➝ Common culprit drugs include allopurinol, anticonvulsants, sulfonamides, antibiotics, and NSAIDs.
➝ Management requires a structured clinical pathway, emphasizing early recognition, immediate drug withdrawal, SCORTEN-based severity assessment, intensive supportive care, and immunomodulatory therapy in selected cases.
➝ In Korea, TEN management is centralized in tertiary hospitals with dermatology, ICU, and burn-unit collaboration.
Why it’s done
→ To stabilize patients rapidly, as mortality risk increases with delayed recognition.
→ To reduce complications such as sepsis, multi-organ failure, and severe ocular/mucosal sequelae.
→ To provide standardized care across hospitals, ensuring timely referral to ICU or burn units.
→ In Korea, TEN pathways improve survival outcomes, minimize long-term disability, and reduce recurrence risk.
Alternatives to a Pathway
→ Ad hoc management: Historically used, but inconsistent and linked to poorer outcomes.
→ Dedicated clinical pathway: Ensures uniform triage, supportive care, and early involvement of multidisciplinary teams.
→ SCORTEN tool: Used globally (and in Korea) to predict prognosis and guide treatment intensity.
Preparation
→ Immediate recognition of early signs: fever, malaise, painful skin, mucosal erosions, flaccid blisters, and widespread epidermal detachment.
→ Medication review: Identify and stop suspected culprit drugs immediately.
→ Baseline investigations: CBC, renal/liver function, electrolytes, blood glucose, arterial blood gas, chest X-ray, and cultures.
→ In Korea, electronic health alerts flag high-risk drugs (e.g., allopurinol without HLA-B*58:01 screening).
How it’s Done – TEN Pathway
Step 1: Immediate Actions
→ Stop culprit medication(s) immediately.
→ Admit to hospital (ICU or burn unit for >10% BSA).
→ Initiate infection control precautions.
Step 2: SCORTEN Severity Assessment (within 24 hours)
→ Age >40 years.
→ Presence of malignancy.
→ Heart rate >120 bpm.
→ BSA detached >10%.
→ Serum urea >10 mmol/L.
→ Serum bicarbonate <20 mmol/L.
→ Serum glucose >14 mmol/L.
→ Mortality rises sharply with each additional risk factor.
Step 3: Supportive Care (Cornerstone of Therapy)
→ Fluid and electrolyte management (similar to burn protocols).
→ Nutrition: high-protein, high-calorie diet or enteral feeding.
→ Wound care: non-adhesive dressings, sterile environment.
→ Temperature regulation in warm rooms to prevent hypothermia.
→ Pain control with opioids or neuropathic pain agents.
→ Strict infection monitoring and antibiotic stewardship (no prophylactic antibiotics).
Step 4: Systemic/Immunomodulatory Therapy (Selected Cases)
→ Corticosteroids: controversial, but used in early severe disease in some Korean centers.
→ Cyclosporine: increasingly used; shown to reduce mortality by inhibiting T-cell activation.
→ IVIG: used variably, particularly in children or severe overlap cases.
→ Biologics (emerging): TNF-α inhibitors and JAK inhibitors are under study.
Step 5: Multidisciplinary Involvement
→ Dermatology: lead diagnosis and skin care.
→ Ophthalmology: urgent evaluation to prevent blindness.
→ ENT/urology/gynecology: mucosal management.
→ ICU/burn unit team: systemic stabilization.
Step 6: Long-Term Care
→ Monitor for scarring, nail loss, pigmentary changes.
→ Ophthalmology follow-up for dry eye, corneal damage, or symblepharon.
→ Psychological support for trauma and anxiety.
→ Documentation of culprit drug allergy in national medical record system.
Recovery
→ Acute stabilization usually achieved in 2–4 weeks.
→ Skin regrows but may leave scarring and pigment changes.
→ Ocular, oral, and genital mucosa may have long-term complications.
→ Mortality depends on SCORTEN score and timeliness of care; Korean centers report improved outcomes with rapid ICU/burn unit referral.
Complications
→ Acute: sepsis, pneumonia, multi-organ failure, electrolyte imbalance.
→ Chronic: ocular sequelae (dry eye, corneal blindness), genital adhesions, nail dystrophy, pigmentation changes, psychological trauma.
→ Treatment-related: risks of systemic steroids (infection), cyclosporine (renal toxicity), IVIG (thrombosis risk).
Treatment Options in Korea
→ Korea follows structured TEN pathways in major hospitals, using SCORTEN-based triage.
→ ICU and burn-unit referrals are standard for severe cases, with dermatology as lead.
→ Cyclosporine is increasingly used in Korean centers, often preferred over corticosteroids alone.
→ HLA-B*58:01 screening is mandatory before allopurinol, reducing TEN incidence significantly.
→ Hospitals use electronic drug safety alerts to prevent re-exposure.
→ Patients receive integrated rehabilitation, including wound healing, ocular care, and psychological support.
→ With Korea’s structured approach, outcomes are among the best globally, with lower recurrence and improved survival.