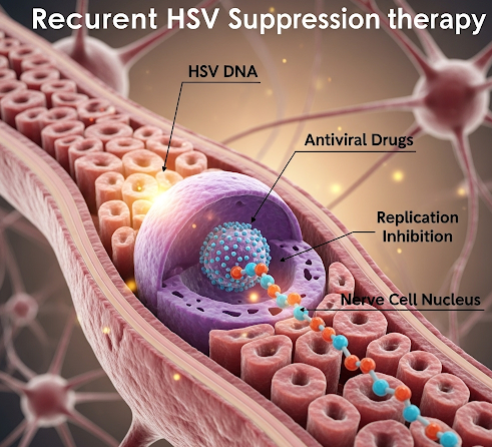
What it is
➝ Recurrent herpes simplex virus (HSV) infection refers to repeated outbreaks of either oral herpes (HSV-1) or genital herpes (HSV-2).
➝ Symptoms include painful blisters, ulcers, burning, and itching, often triggered by stress, illness, or hormonal changes.
➝ Suppressive therapy involves taking antiviral medications daily or long-term to reduce outbreak frequency, severity, and viral shedding.
➝ In Korea, recurrent HSV suppression is widely practiced in dermatology, gynecology, and infectious disease clinics, using structured antiviral regimens and patient education.
Why it’s done
→ To reduce recurrence frequency, especially in patients with more than 6 outbreaks per year.
→ To lessen outbreak severity and shorten duration when flare-ups occur.
→ To reduce asymptomatic viral shedding, lowering the risk of transmission to sexual partners.
→ To improve quality of life, as frequent HSV outbreaks can cause social, psychological, and sexual distress.
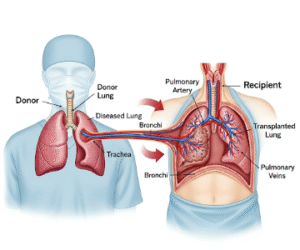
→ In immunocompromised patients, suppression helps prevent serious complications like disseminated HSV or keratitis.
Alternatives
→ Episodic therapy: Antivirals taken only at outbreak onset (effective but less preventive).
→ Topical antivirals: Less effective than systemic therapy.
→ Lifestyle and trigger management: Stress reduction, adequate sleep, avoiding excessive sun exposure.
→ Preventive measures: Condom use, avoiding direct contact during outbreaks, partner testing.
→ Vaccines: Still in research; not yet available in clinical practice.
Preparation
→ Diagnosis is confirmed through PCR, culture, or serology if unclear.
→ Baseline evaluation includes renal function in older adults or those with comorbidities, since antivirals are renally excreted.
→ Patient counseling about daily medication adherence and safe sex practices is critical.
→ In Korea, many clinics provide education booklets and mobile reminders to improve adherence.
How it’s Done
→ First-line suppressive therapy:
- Acyclovir: 400 mg orally twice daily.
- Valacyclovir: 500 mg once daily (for patients with <10 recurrences/year) or 1 g once daily (for frequent recurrences).
- Famciclovir: 250 mg twice daily (alternative).
→ Duration: Typically 6–12 months, followed by reassessment. Long-term therapy may continue if outbreaks recur after stopping.
→ Episodic therapy option (if not on daily suppression): Higher-dose antivirals at first sign of outbreak, started within 24 hours.
→ In Korea, suppression protocols are often tailored based on outbreak frequency, lifestyle, and partner transmission concerns.
Recovery
→ Most patients experience 70–80% fewer outbreaks on suppressive therapy.
→ Outbreaks that occur are usually milder, shorter, and less painful.
→ Patients report improved confidence, intimacy, and reduced stigma with effective suppression.
→ Long-term adherence helps reduce the psychological burden of recurrent HSV.
Complications
→ Medication side effects: Headache, nausea, mild GI upset. Rare kidney toxicity with acyclovir if hydration is poor.
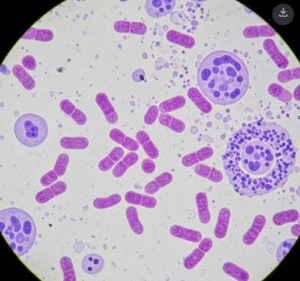
→ Resistance: Rare in immunocompetent patients, but possible in immunosuppressed individuals.
→ Rebound outbreaks: Symptoms may return once suppression is stopped.
→ Adherence challenges: Daily therapy may be difficult for some patients, requiring counseling and follow-up.
Treatment Options in Korea
→ Korean clinics frequently use valacyclovir for suppression due to convenient once-daily dosing and strong evidence for transmission reduction.
→ Acyclovir is also widely used, especially in patients requiring cost-effective options.
→ Many hospitals integrate sexual health counseling and partner education with HSV suppression plans.
→ In high-risk patients (immunocompromised, transplant recipients), long-term suppressive therapy is strongly emphasized.
→ Korea also promotes digital adherence tools, such as mobile apps and hospital reminder systems, to support consistent medication use.
→ With Korea’s structured and modern approach, recurrent HSV suppression therapy helps patients achieve fewer outbreaks, better quality of life, and reduced transmission risk.