What it is
➝ Prurigo nodularis (PN) is a chronic, relapsing, neuro-inflammatory skin disorder defined by intensely itchy, firm nodules typically located on the arms, legs, trunk, and sometimes the scalp.
➝ It arises from a self-perpetuating itch–scratch cycle: scratching induces inflammation, which thickens the skin into nodules, which then cause more itching.
➝ Histologically, PN shows hyperkeratosis, acanthosis, nerve fiber proliferation, mast cell infiltration, and increased IL-4/IL-31 activity, linking it to atopic dermatitis and other systemic conditions.
➝ It is strongly associated with atopy, chronic renal disease, liver disease, thyroid dysfunction, HIV, neuropathic disorders, and psychiatric comorbidities.
➝ In Korea, PN is treated in dermatology and allergy-immunology centers, often with integrated care across dermatology, neurology, psychiatry, and internal medicine.
Why it’s done
→ PN patients suffer from severe chronic pruritus that disrupts sleep and daily life.
→ Uncontrolled PN leads to lichenified nodules, excoriations, scarring, and secondary infections.
→ Long-term, PN can cause pigmentary changes, disfigurement, anxiety, and depression.
→ Management is therefore aimed at breaking the itch–scratch cycle, reducing inflammation and neural sensitization, preventing new nodule formation, improving cosmetic appearance, and addressing systemic associations and psychiatric impact.
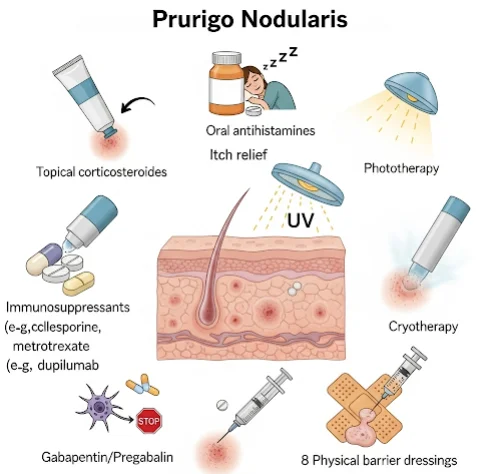
Alternatives / Stepwise Treatment Strategy
General measures
→ Liberal use of thick emollients, ceramide creams, or ointments to restore barrier function.
→ Cold compresses or menthol/pramoxine lotions to soothe itch.
→ Behavioral strategies: keep nails short, wear cotton gloves at night, avoid scratching triggers.
→ In Korea, patients are educated through visual tools, digital apps, and clinic handouts.
Topical therapy
→ High-potency corticosteroids (e.g., clobetasol, betamethasone) often under occlusion (plastic wrap, hydrocolloid dressing).
→ Calcineurin inhibitors (tacrolimus, pimecrolimus) used on face, flexures, or as maintenance.
→ Topical capsaicin, pramoxine, or lidocaine for neuropathic itch nodules.
→ Topical vitamin D analogues or keratolytics occasionally for chronic hyperkeratotic nodules.
Intralesional therapy
→ Triamcinolone acetonide injections (5–10 mg/mL) into thick nodules reduce bulk, redness, and itch.
→ In Korea, often combined with fractional CO₂ laser or cryotherapy for resistant nodules.
Systemic therapy
→ Antihistamines: non-sedating by day, sedating at night for itch control and sleep improvement.
→ Gabapentin or pregabalin: reduce neuropathic itch signals.
→ Antidepressants (mirtazapine, amitriptyline, doxepin): helpful for itch modulation and sleep disturbance.
→ Immunosuppressants:
- Cyclosporine: effective, but requires monitoring (renal, BP).
- Methotrexate: useful for extensive or refractory PN.
- Thalidomide/lenalidomide: potent, but restricted due to neuropathy/teratogenicity risks.
→ Biologics (new, advanced therapies): - Dupilumab: IL-4Rα inhibitor, already used in atopic dermatitis, approved for PN in many countries and available in Korea.
- Nemolizumab: IL-31 receptor antibody, highly effective against itch; in late-stage trials and compassionate use in Korea.
- JAK inhibitors (upadacitinib, baricitinib, tofacitinib): promising results in PN patients resistant to other therapies.
Phototherapy
→ Narrowband UVB: reduces itch and inflammation; often first-line systemic-sparing option in Korea.
→ Excimer laser: targeted for localized resistant nodules.
Preparation
→ Detailed history and exam: duration of itch, number/location of nodules, comorbidities, systemic symptoms.
→ Laboratory tests: CBC, renal/liver function, thyroid panel, HIV/hepatitis screening if indicated.
→ Psychological screening: anxiety, depression, obsessive scratching behaviors.
→ In Korea, clinics often use Itch Numeric Rating Scale (NRS), Visual Analogue Scale (VAS), and DLQI (Dermatology Life Quality Index) for baseline assessment.
→ Digital photography and dermoscopy are used to track lesion regression during treatment.
How it’s Done
→ Step 1: Initiate emollients, potent topical corticosteroids under occlusion, and antihistamines.
→ Step 2: For resistant nodules, add intralesional steroid injections or topical calcineurin inhibitors, sometimes combined with cryotherapy or fractional laser.
→ Step 3: If uncontrolled, escalate to systemic therapy (gabapentin, pregabalin, cyclosporine, methotrexate). Phototherapy if widespread.
→ Step 4: Severe or refractory PN may be treated with biologics (dupilumab, nemolizumab) or JAK inhibitors.
→ Step 5: Maintenance with calcineurin inhibitors, moisturizers, and behavioral reinforcement once nodules flatten.
→ In Korea, treatment often follows multimodal combination protocols, targeting inflammation, itch signaling, and psychological reinforcement simultaneously.
Recovery
→ Initial itch reduction may be achieved within 2–4 weeks of starting therapy.
→ Nodules begin to flatten over 6–12 weeks, though pigmentation and thickened skin may take months to normalize.
→ Biologics (dupilumab, nemolizumab) show rapid itch relief (within days to weeks), with nodular regression over months.
→ Patients report improved sleep, concentration, and emotional well-being with effective therapy.
Complications
→ Persistent lesions if itch–scratch cycle is not broken.
→ Scarring, hypopigmentation, or hyperpigmentation from chronic scratching.
→ Secondary bacterial infection from excoriations.
→ Drug-related side effects:
- Cyclosporine: hypertension, nephrotoxicity.
- Methotrexate: hepatotoxicity, bone marrow suppression.
- Thalidomide: neuropathy, teratogenicity.
→ Psychological impact: depression and anxiety if disease remains uncontrolled.
Treatment Options in Korea
→ Korean dermatology centers manage PN using a tiered, stepwise protocol: topical therapy → intralesional injections → systemic therapy → biologics/phototherapy.
→ Dupilumab is increasingly prescribed for refractory PN, especially in patients with overlapping atopic dermatitis.
→ Clinical trials in Korea are investigating nemolizumab and JAK inhibitors for PN, providing access for resistant cases.
→ Phototherapy units (NB-UVB, excimer) are widely available in hospitals and specialty dermatology clinics.
→ Clinics often combine ablative fractional laser (for drug-assisted delivery of steroids or 5-FU) with systemic therapy for stubborn nodules.
→ Psychological support and stress management are routinely incorporated, as scratching behavior is often exacerbated by emotional triggers.