What it is
→ Photodynamic therapy (PDT) for the face is a non-invasive dermatological treatment that uses a combination of a photosensitizing agent (a special cream or solution) and controlled light exposure to selectively destroy damaged or abnormal skin cells.
→ When the photosensitizer is applied to the skin, it is absorbed by precancerous, sun-damaged, or acne-prone cells. Once activated by a specific wavelength of light, the agent produces reactive oxygen molecules that kill the targeted cells.
→ PDT is widely used to treat:
- Actinic keratoses (precancerous sun-damaged spots).
- Acne vulgaris (by targeting overactive sebaceous glands and bacteria).
- Superficial skin cancers (in certain cases).
- Photoaging signs (fine wrinkles, pigmentation, and uneven tone).
→ On the face, PDT is particularly effective because facial skin is often sun-exposed and prone to both cosmetic and medical skin conditions.
Why it’s done
→ Photodynamic therapy on the face is performed for both medical and cosmetic reasons:
- To eliminate precancerous lesions before they progress to squamous cell carcinoma.
- To reduce chronic sun damage and actinic keratoses across broad facial areas.
- To improve cosmetic appearance by reducing pigmentation, redness, and wrinkles.
- To treat acne and oily skin, reducing inflammation and future breakouts.
- To provide a non-surgical, minimally invasive option with shorter downtime than aggressive procedures.
→ Patients with fair skin, long-term sun exposure, or recurring precancerous spots benefit most from facial PDT.
Alternatives
→ Alternatives to PDT for the face include:
- Topical therapies → 5-FU cream, imiquimod, or retinoids for actinic keratoses and acne.
- Cryotherapy → freezing individual lesions with liquid nitrogen.
- Laser therapy → fractional CO₂, erbium, or IPL for pigmentation and wrinkles.
- Chemical peels → exfoliating agents to remove damaged layers of skin.
- Oral acne medications → antibiotics, isotretinoin, or hormonal therapy.
→ These alternatives may be chosen depending on severity, patient preference, and tolerance to PDT.
Preparation
→ Proper preparation ensures effective and safe PDT:
- Dermatology consultation → to determine if PDT is suitable.
- Avoid sun exposure → at least 1–2 weeks prior to treatment.
- Stop photosensitizing drugs (if prescribed) → some medications increase sensitivity to light.
- No tanning or aggressive skincare → discontinue retinoids, peels, or exfoliants several days before.
- Clean skin → arrive with no makeup, sunscreen, or lotions.
- Protective planning → bring sunglasses, hats, and sunscreen for post-treatment care.
How it’s Done
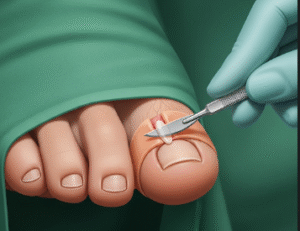
→ A PDT session for the face typically involves:
- Application of photosensitizer → cream (such as aminolevulinic acid or methyl aminolevulinate) applied to the face.
- Incubation period → 30–120 minutes, allowing the cream to be absorbed by abnormal cells.
- Light activation → dermatologist shines a controlled wavelength of light (blue, red, or IPL) onto the face.
- Reaction phase → the activated photosensitizer destroys damaged or abnormal cells.
- Post-treatment care → sunscreen and soothing ointments are applied immediately afterward.
→ A session usually lasts 1.5–3 hours, including incubation and light exposure.
Recovery
→ Recovery from facial PDT is relatively short compared to surgical treatments:
- Day 1–3 → redness, burning, and mild swelling similar to a sunburn.
- Day 3–7 → peeling, crusting, and flaking as damaged skin sheds.
- Day 7–14 → skin heals, revealing smoother texture and improved tone.
→ Patients should:
- Avoid direct sun exposure for at least 48 hours.
- Apply soothing ointments and fragrance-free moisturizers.
- Use broad-spectrum sunscreen daily.
- Follow dermatologists’ instructions strictly for aftercare.
→ Most people return to normal activities in 2–5 days, with complete recovery in about 1–2 weeks.
Complications
→ PDT is generally safe, but temporary side effects can include:
- Redness, swelling, or stinging during and after treatment.
- Peeling and dryness during recovery.
- Crusting or scabbing on treated areas.
- Temporary hyperpigmentation or hypopigmentation, more common in darker skin tones.
- Photosensitivity reactions if exposed to sunlight too soon.
→ Rare complications: infection, scarring, or persistent discoloration.
→ With professional care and strict sun protection, complications are minimal.
Treatment options in Korea
→ Korea is a global leader in dermatology and offers advanced PDT treatments for the face:
- Cutting-edge clinics → Seoul, Busan, and Daegu host clinics equipped with the latest PDT devices.
- Customized protocols → Korean dermatologists often combine PDT with topical therapies, chemical peels, or lasers for enhanced results.
- Medical–cosmetic integration → clinics focus on both medical lesion clearance and cosmetic rejuvenation.
- High patient safety → Korea emphasizes strict aftercare protocols and close follow-up.
- AI-supported imaging → some clinics use digital skin analysis to track improvements before and after PDT.
- Popular use for acne → PDT is widely performed in Korea for acne-prone skin, with long-lasting results.
- International patient services → English-speaking dermatologists and global healthcare support make PDT highly accessible to medical tourists.
→ With its advanced technology, aesthetic expertise, and preventive approach, Korea is one of the best destinations for facial photodynamic therapy.