What it is
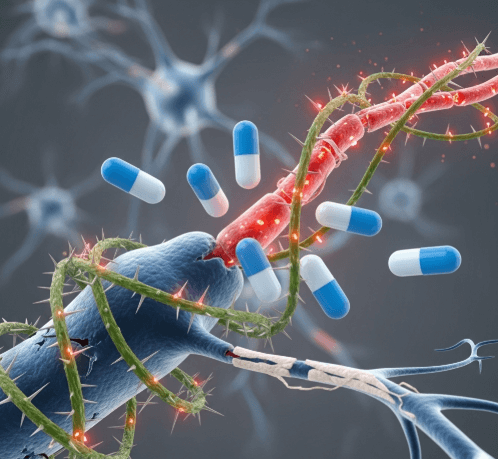
➝ Neuropathic itch is chronic pruritus caused by damage or dysfunction of the peripheral or central nervous system, rather than skin inflammation.
➝ It can occur in conditions such as post-herpetic neuralgia, notalgia paresthetica, brachioradial pruritus, diabetic neuropathy, multiple sclerosis, stroke, or spinal cord disease.
➝ Gabapentinoids (gabapentin and pregabalin) are anticonvulsant drugs that modulate calcium channels in neurons, reducing abnormal excitability and transmission of itch signals.
➝ In Korea, gabapentinoids are widely used in dermatology, neurology, and pain clinics for chronic neuropathic itch syndromes.
Why it’s done
→ To relieve intense, treatment-resistant itching that does not respond to antihistamines or topical steroids.
→ To improve sleep and quality of life, since neuropathic itch is often worse at night.
→ To prevent secondary skin damage (excoriations, lichenification, scarring) from scratching.
→ To manage itch in complex systemic or neurological conditions where standard dermatologic treatments fail.
Alternatives
→ Topical therapies: capsaicin, lidocaine patches, pramoxine, menthol.
→ Antidepressants: mirtazapine, amitriptyline, doxepin.
→ Opioid modulators: naltrexone, butorphanol in selected refractory cases.
→ Phototherapy: NB-UVB, excimer laser for localized neuropathic itch.
→ Biologics/JAK inhibitors: mainly for inflammatory itch, less effective in pure neuropathic syndromes.
Preparation
→ Detailed history and exam to confirm neuropathic cause of itch (burning, tingling, localized distribution, association with neurological disease).
→ Baseline labs (renal and liver function) since gabapentinoids are renally excreted.
→ Patient counseling about gradual titration, possible drowsiness, dizziness, and need for long-term use.
→ In Korea, physicians often perform neurology consultation and imaging (MRI spine/brain) if structural pathology is suspected.
How it’s Done
→ Gabapentin
- Start: 100–300 mg at night.
- Titrate slowly every 3–7 days.
- Typical dose: 900–1800 mg/day in divided doses (sometimes up to 3600 mg).
→ Pregabalin
- Start: 25–50 mg at night.
- Increase to 75–150 mg twice daily.
- Usual range: 150–300 mg/day; max 600 mg/day if tolerated.
→ Both drugs are given orally and require gradual dose escalation to reduce side effects.
→ Combination with topical therapy (capsaicin, lidocaine) is common for localized itch.
→ In Korea, physicians often prescribe pregabalin more frequently due to its predictable absorption and simpler dosing schedule.
Recovery
→ Patients often notice partial relief within 1–2 weeks, with maximum effect after 4–6 weeks of titration.
→ Neuropathic itch intensity may decrease by 50–70%, improving sleep and mood.
→ Long-term therapy is usually required, with dose adjustments depending on recurrence.
Complications
→ Common side effects: drowsiness, dizziness, unsteadiness, peripheral edema, weight gain.
→ Rare: blurred vision, mood changes, withdrawal symptoms if stopped abruptly.
→ Elderly patients: higher risk of sedation and falls, requiring cautious dosing.
→ Requires dose adjustment in renal impairment.
Treatment Options in Korea
→ Korean dermatology and neurology clinics widely prescribe gabapentin and pregabalin as standard therapy for neuropathic itch.
→ Pregabalin is often favored for brachioradial pruritus, notalgia paresthetica, and post-herpetic neuralgia, while gabapentin is used for widespread or systemic neuropathic itch.
→ Major hospitals integrate gabapentinoids with physical therapy, phototherapy, or topical anesthetics for multimodal management.
→ Patients are monitored closely for side effects, especially elderly individuals, with regular follow-ups every 4–8 weeks.
→ Korean clinical practice emphasizes patient education and gradual titration, ensuring adherence and minimizing risks.