What it is
➝ Mastocytosis is a rare disorder characterized by an abnormal accumulation of mast cells in the skin and/or internal organs.
➝ Cutaneous mastocytosis typically presents with brownish patches, hives, or urticaria pigmentosa, often accompanied by itching, flushing, or blistering.
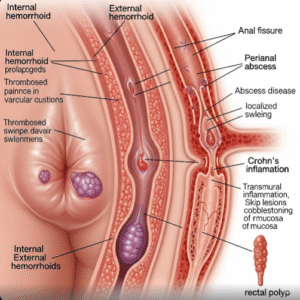
➝ Systemic mastocytosis involves mast cell infiltration of bone marrow, liver, spleen, or GI tract and can cause anaphylaxis, abdominal pain, diarrhea, or bone pain.
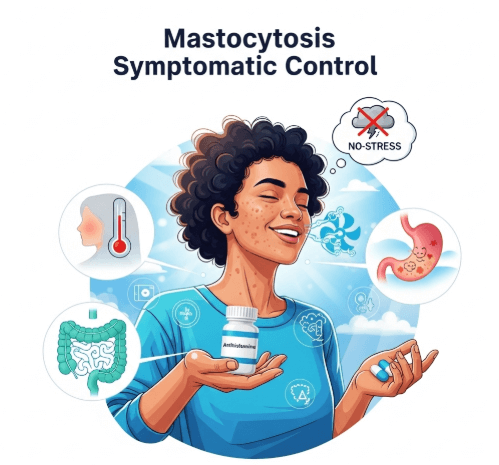
➝ Since mastocytosis cannot usually be cured, management focuses on symptomatic control and prevention of triggers that activate mast cells.
➝ In Korea, treatment emphasizes antihistamines, mast cell stabilizers, and patient education as part of long-term management.
Why it’s done
→ To relieve itching, flushing, and hives, which affect quality of life.
→ To prevent anaphylactic reactions triggered by foods, insect stings, medications, or stress.
→ To control gastrointestinal symptoms such as abdominal pain, diarrhea, and nausea caused by mast cell mediator release.
→ To manage systemic complications like bone pain, fatigue, and hypotension.
→ In Korea, symptomatic control is considered essential because mastocytosis can be chronic and unpredictable.
Alternatives / Symptom Control Approaches
→ Antihistamines
- H1 blockers (cetirizine, loratadine, fexofenadine) for itching, flushing, hives.
- H2 blockers (ranitidine, famotidine) for gastric acid overproduction and reflux.
→ Mast cell stabilizers
- Cromolyn sodium (oral solution) to reduce gastrointestinal symptoms.
→ Leukotriene receptor antagonists
- Montelukast or zafirlukast may help with flushing, abdominal symptoms, or asthma-like complaints.
→ Corticosteroids
- Short courses for severe skin flares, but not recommended long-term.
→ Epinephrine auto-injector
- For patients at risk of anaphylaxis.
→ Adjunctive care
- Phototherapy (PUVA, narrowband UVB) in cutaneous mastocytosis.
- Pain management for bone or muscle involvement.
Preparation
→ Careful history-taking to identify triggers: alcohol, spicy foods, temperature changes, insect stings, NSAIDs, opioids, or contrast dyes.
→ Baseline workup: serum tryptase levels, complete blood count, and organ function tests in suspected systemic disease.
→ Patient education is critical before starting therapy: learning to avoid triggers and understanding emergency plans for anaphylaxis.
→ In Korea, patients are often enrolled in specialized allergy or hematology clinics for structured care.
How it’s Done
→ Daily H1 antihistamine: First-line for skin itching, flushing, and urticaria.
→ Add H2 antihistamine if gastric acid symptoms are present.
→ Cromolyn sodium is added for GI symptoms, taken before meals.
→ Montelukast may be introduced for persistent symptoms.
→ Epinephrine auto-injector is prescribed for patients with systemic mastocytosis or anaphylaxis history.
→ Lifestyle and trigger avoidance:
- Avoid sudden temperature changes, hot showers, or friction on lesions.
- Avoid aspirin, NSAIDs, and alcohol, which often worsen symptoms.
- Use gentle skincare and fragrance-free moisturizers.
→ In Korea, doctors often recommend structured stepwise medication escalation and provide patients with personalized emergency kits.
Recovery
→ Itching, flushing, and skin lesions usually improve within days to weeks on antihistamines.
→ GI symptoms often stabilize after 2–4 weeks of cromolyn sodium.
→ Patients report improved daily comfort, sleep quality, and confidence once symptoms are under control.
→ Long-term remission is rare, but symptom stability and prevention of severe reactions are achievable goals.
Complications
→ Uncontrolled mastocytosis: persistent itching, flushing, GI distress, bone pain, or recurrent anaphylaxis.
→ Medication-related:
- Antihistamines may cause mild drowsiness.
- Cromolyn sodium may cause diarrhea or bloating.
- Corticosteroids carry long-term side effects if overused.
→ Psychological burden: chronic unpredictability of symptoms often leads to anxiety.
Treatment Options in Korea
→ Korean dermatology and allergy clinics commonly use second-generation H1 antihistamines as first-line therapy, often at higher doses for resistant cases.
→ Combination therapy (H1 + H2 blockers, cromolyn sodium, montelukast) is available and tailored to patient symptoms.
→ Epinephrine auto-injectors are prescribed for systemic mastocytosis, with education sessions on proper use.
→ Hospitals with hematology departments manage systemic cases with advanced treatments such as interferon-alpha or tyrosine kinase inhibitors in rare aggressive disease.
→ Patient education programs in Korea emphasize trigger avoidance, safe medication use, and lifestyle modifications.
→ With Korea’s multidisciplinary approach, patients benefit from integrated care combining dermatology, allergy, hematology, and lifestyle guidance, ensuring effective symptomatic control.