What it is
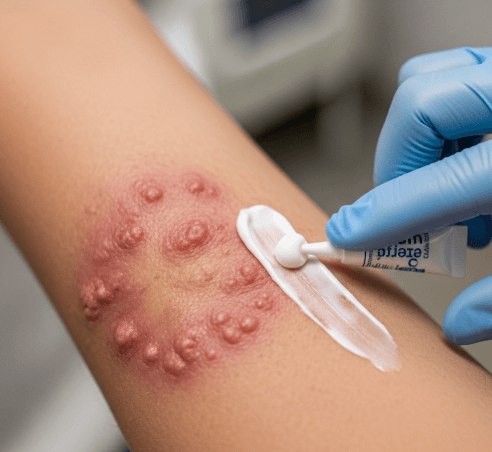
➝ Majocchi granuloma is a deep fungal infection of the skin and hair follicles, most often caused by dermatophytes such as Trichophyton rubrum.
➝ Unlike superficial ringworm, the fungus penetrates the dermis and hair follicles, leading to red, inflamed nodules, papules, and pustules, often on the legs, arms, or face.
➝ It commonly occurs in immunosuppressed individuals, people with chronic steroid use, or after trauma/shaving that allows fungus to invade deeper layers.
➝ Because the infection is deep-seated, topical antifungals are insufficient. Systemic antifungal therapy is the mainstay of treatment.
Why it’s done
→ To eradicate the deep fungal infection and prevent spread.
→ To avoid chronic or recurrent disease, as untreated Majocchi granuloma does not resolve spontaneously.
→ To reduce pain, swelling, and discomfort, since lesions may mimic bacterial folliculitis or abscesses.
→ To prevent scarring and pigmentation changes that can result from prolonged inflammation.
→ In Korea, therapy is focused on systemic antifungal treatment combined with supportive skin care, with careful diagnosis to distinguish it from bacterial infections.
Alternatives
→ Topical antifungals: Helpful as adjunct therapy but not effective alone due to the depth of infection.
→ Systemic antifungals (mainstay):
- Terbinafine: First-line, excellent activity against dermatophytes.
- Itraconazole: Commonly used, especially if terbinafine is not tolerated.
- Fluconazole: Alternative option.
- Griseofulvin: Less common now but still effective in some cases.
→ Antibiotics: Only used if secondary bacterial infection is confirmed, not as primary therapy.
→ Steroid withdrawal: If triggered by inappropriate topical corticosteroid use, discontinuing steroids is essential.
Preparation
→ Dermatologist performs skin scraping, fungal culture, or biopsy to confirm diagnosis, since it can resemble bacterial folliculitis.
→ Baseline tests may include liver function and kidney function if systemic antifungals are planned.
→ Patients are advised to:
- Stop using topical corticosteroids on affected areas.
- Maintain proper hygiene and skin care.
- Avoid shaving over active lesions until cleared.
→ In Korea, diagnosis is usually confirmed with direct microscopy (KOH test) and, if needed, histopathology.
How it’s Done
→ Terbinafine: 250 mg daily for 4–6 weeks.
→ Itraconazole: 100–200 mg daily for 4–6 weeks, or pulse dosing (200 mg twice daily for 1 week/month).
→ Fluconazole: 150–300 mg once weekly for several weeks in selected cases.
→ Topical antifungal cream may be added to reduce surface fungal load.
→ Supportive care includes gentle cleansing, avoiding occlusive ointments, and using soothing moisturizers.
→ In Korea, systemic therapy is often combined with adjunctive laser or light-based therapies to speed healing and reduce pigmentation changes.
Recovery
→ Improvement in redness, swelling, and pustules is often seen within 2–3 weeks of therapy.
→ Complete clearance usually requires 4–8 weeks of treatment, depending on severity.
→ Recurrence risk is minimized with full treatment completion and preventive hygiene.
→ Patients typically regain normal skin texture, though post-inflammatory pigmentation may take months to fade.
Complications
→ If untreated: Infection may persist for months, leading to scarring and chronic inflammation.
→ Medication-related risks:
- Terbinafine: Rare liver toxicity, taste changes.
- Itraconazole: Drug interactions, liver function changes.
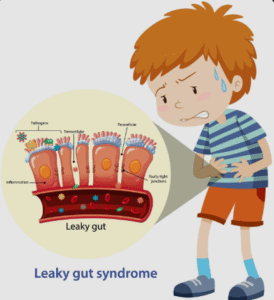
- Fluconazole: Gastrointestinal upset, rare liver issues.
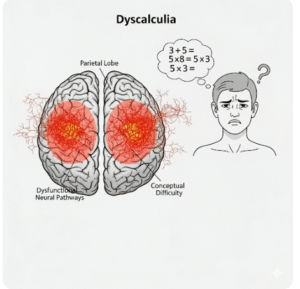
→ Misdiagnosis: Treated as bacterial folliculitis instead of fungal infection, leading to worsening with antibiotics or steroids.
Treatment Options in Korea
→ Korean dermatologists are highly experienced in diagnosing atypical fungal infections like Majocchi granuloma.
→ Standard therapy includes oral terbinafine or itraconazole, often guided by culture results.
→ Topical antifungals are used alongside systemic drugs to reduce recurrence.
→ Clinics provide regular follow-up with blood tests for patients on systemic antifungals.
→ Some dermatology centers in Korea integrate laser treatments or chemical peels after infection clearance to address pigmentation or scarring.
→ Patient education focuses on avoiding corticosteroid misuse, proper shaving techniques, and antifungal hygiene practices to prevent recurrence.