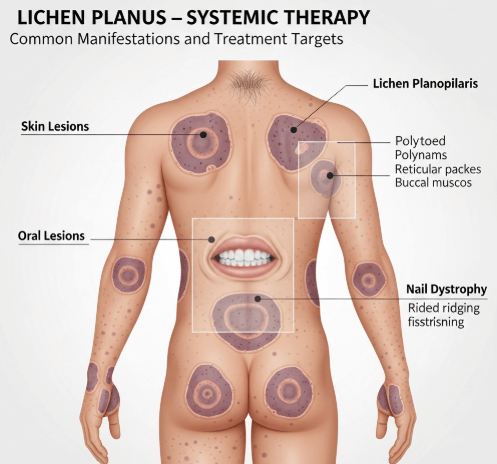
What it is
➝ Lichen planus (LP) is a chronic, inflammatory skin and mucosal disease involving the immune-mediated attack on keratinocytes.
➝ It presents with purple, polygonal, pruritic, planar papules and plaques on the skin, as well as oral, genital, scalp (lichen planopilaris), and nail involvement.
➝ While many cutaneous cases resolve within 1–2 years, mucosal, nail, and hair follicle disease can be severe, chronic, and scarring, requiring systemic therapy.
➝ In Korea, systemic treatment is reserved for extensive, resistant, or disabling lichen planus, combining immunosuppressive and immunomodulatory approaches.
Why it’s done
→ To control severe itching, burning, or pain that disrupts daily life.
→ To prevent scarring alopecia in lichen planopilaris or permanent nail loss.
→ To reduce oral/genital discomfort that interferes with eating, intimacy, and quality of life.
→ To limit the psychosocial burden, since visible skin lesions often cause anxiety and stigma.
→ In Korea, systemic therapy is used when topical corticosteroids, calcineurin inhibitors, or phototherapy are insufficient.
Alternatives
→ Topical corticosteroids: First-line for limited cutaneous and mucosal LP.
→ Intralesional corticosteroids: For hypertrophic plaques or nail matrix disease.
→ Phototherapy (NB-UVB or PUVA): Useful for widespread cutaneous LP.
→ Systemic therapy: Required for severe, refractory, or scarring forms.
Preparation
→ Confirm diagnosis with clinical examination and skin/mucosal biopsy.
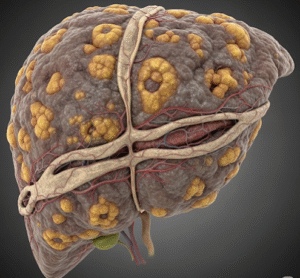
→ Baseline blood tests: complete blood count, liver and kidney function, hepatitis screening (since LP is sometimes associated with hepatitis C).
→ Review comorbidities and risk factors before choosing systemic therapy.
→ In Korea, dermatology clinics often perform baseline digital photography to track treatment response.
How it’s Done – Systemic Therapy Options
→ Oral corticosteroids
- Prednisone 0.5–1 mg/kg/day tapered over weeks.
- Used for acute, severe flares but not suitable long-term due to side effects.
→ Immunosuppressive agents
- Azathioprine: Effective for mucosal LP.
- Mycophenolate mofetil: Useful in refractory cases.
- Methotrexate: Sometimes used in lichen planopilaris and nail LP.
- Cyclosporine: Rapid relief in resistant LP but requires monitoring.
→ Retinoids
- Acitretin: Beneficial for hypertrophic LP and widespread disease.
→ Biologic therapy (emerging)
- Case reports support dupilumab and JAK inhibitors in resistant LP, though not yet standard.
→ Adjunctive measures
- Antihistamines for itching.
- Pain control for oral/genital erosive lesions.
- Gentle skincare and barrier protection.
→ In Korean practice, systemic corticosteroids are often used for short induction, followed by steroid-sparing agents such as azathioprine or cyclosporine.
Recovery
→ With systemic therapy, skin lesions often flatten within 4–8 weeks, though pigmentation may linger.
→ Oral and genital LP may take several months to improve.
→ Hair and nail disease require early aggressive treatment to prevent irreversible damage.
→ Long-term remission is possible, but relapse is common, requiring maintenance or retreatment.
Complications
→ Uncontrolled LP: Scarring alopecia, nail dystrophy, strictures in mucosal disease.
→ Medication-related:
- Corticosteroids: weight gain, osteoporosis, diabetes, hypertension.
- Azathioprine: bone marrow suppression, hepatotoxicity.
- Cyclosporine: nephrotoxicity, hypertension, gum hyperplasia.
- Acitretin: dryness, teratogenicity.
→ Psychological impact: Disfigurement and chronic pain can lead to anxiety and depression.
Treatment Options in Korea
→ Korean dermatology clinics follow an escalation model:
- Start with high-potency topical steroids and/or phototherapy.
- Add systemic corticosteroids for severe acute disease.
- Switch to steroid-sparing immunosuppressants (azathioprine, cyclosporine, methotrexate) for long-term control.
→ Oral and genital LP are often co-managed with oral medicine, gynecology, or urology specialists for comprehensive care.
→ Acitretin is available and used in resistant hypertrophic or widespread LP.
→ Some advanced centers are exploring dupilumab and JAK inhibitors for refractory LP under clinical programs.
→ Patient education in Korea emphasizes avoiding skin trauma (Koebner phenomenon), maintaining oral hygiene, and consistent follow-up.
→ With Korea’s multidisciplinary care, systemic therapy for LP is delivered in a personalized, closely monitored approach, improving outcomes and minimizing complications.