What it is
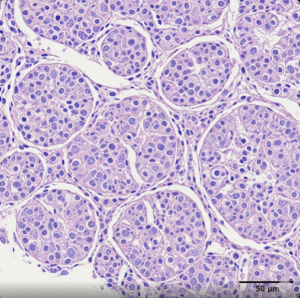
➝ Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe mucocutaneous reactions, most often triggered by medications, with high mortality and long-term sequelae.
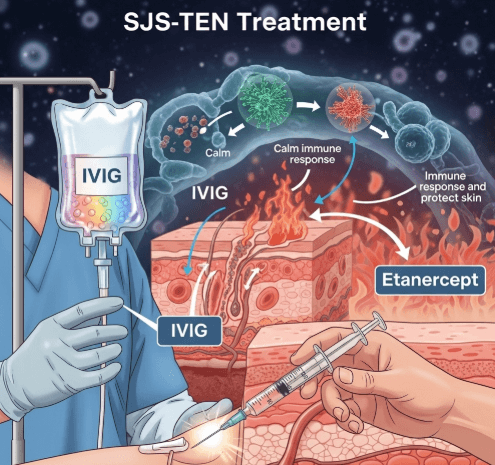
➝ IVIG (intravenous immunoglobulin) and etanercept (TNF-α inhibitor) are immunomodulatory therapies used in specialized centers, aiming to stop disease progression by blocking pathways of keratinocyte apoptosis and inflammation.
➝ In Korea, these treatments are available mainly in tertiary hospitals with dermatology, ICU, and burn-unit support.
Why it’s done
→ To reduce mortality and morbidity in severe SJS/TEN.
→ To shorten time to re-epithelialization and improve recovery.
→ To minimize long-term ocular and mucosal complications.
→ To provide therapeutic options beyond corticosteroids or cyclosporine.
→ In Korea, these therapies are used in center-based structured protocols for selected patients.
Alternatives
→ Supportive ICU/burn unit care: cornerstone of therapy.
→ Systemic corticosteroids: commonly used, though controversial due to infection risk.
→ Cyclosporine: increasingly preferred in many centers for immune suppression.
→ Plasmapheresis or IVIG–steroid combinations: sometimes used in refractory cases.
→ Emerging biologics (e.g., JAK inhibitors, infliximab): experimental.
Preparation
→ Confirm diagnosis and severity with clinical evaluation and SCORTEN scoring.
→ Stop culprit drug immediately.
→ Perform baseline blood tests: CBC, renal, liver function, electrolytes.
→ Exclude active infections or contraindications before initiating immunomodulatory therapy.
→ In Korea, multidisciplinary review is required before IVIG or etanercept initiation.
How it’s Done
→ IVIG: Total dose 2 g/kg divided over 3–5 days, administered intravenously in ICU or burn unit. Mechanism: blocks Fas–FasL mediated apoptosis of keratinocytes. Monitoring includes vitals, renal function, and clotting risk.
→ Etanercept: 50 mg subcutaneous injection, repeated weekly for 1–2 doses depending on severity. Mechanism: inhibits TNF-α signaling, reducing inflammatory cascade and epidermal destruction. Monitoring includes infection screening, CBC, and liver function.
→ Combination approaches: Some Korean centers use etanercept with corticosteroids or IVIG with cyclosporine in complex cases.
Recovery
→ IVIG: may stabilize disease and limit progression, though results vary.
→ Etanercept: clinical studies show faster healing (7–10 days) and lower mortality compared to corticosteroids alone.
→ Patients in Korean centers often achieve shorter hospitalization and improved ocular outcomes with early immunomodulation.
Complications
→ IVIG: infusion reactions, renal dysfunction, thrombosis, high cost.
→ Etanercept: infection risk, potential TB reactivation (screening mandatory in Korea).
→ General SJS/TEN risks: sepsis, multi-organ failure, delayed wound healing.
Treatment Options in Korea
→ IVIG is used in severe TEN with rapid progression or extensive BSA involvement.
→ Etanercept is increasingly favored in Korean tertiary hospitals for its effectiveness in reducing mortality and sequelae.
→ Cyclosporine remains a common option and is often compared alongside etanercept in Korean studies.
→ Multidisciplinary teams decide eligibility, with dermatology, ICU, ophthalmology, and infectious disease specialists working together.
→ National insurance coverage is limited; advanced therapies are typically offered in major university hospitals.