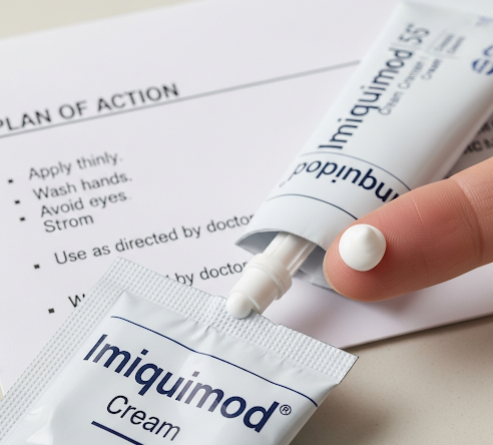
What it is
→ Imiquimod cream is an immune-response modifier used in dermatology to treat several skin conditions, most notably actinic keratoses (precancerous sun-damaged lesions), superficial basal cell carcinoma, and external genital warts.
→ It works by stimulating the body’s innate and adaptive immune system, activating immune cells to attack abnormal or virus-infected skin cells.
→ An Imiquimod cream plan refers to a structured dermatology-guided approach for applying this medication safely and effectively, with monitoring for side effects and long-term outcomes.
→ Unlike destructive treatments (cryotherapy or surgery), imiquimod activates the body’s natural defense system, making it valuable for field treatment across sun-damaged areas.
Why it’s done
→ The main purpose of an Imiquimod cream plan is to:
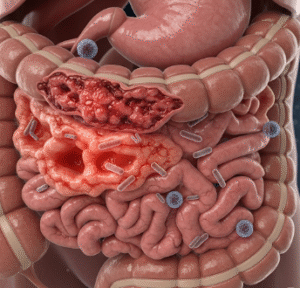
- Treat actinic keratoses and prevent progression to squamous cell carcinoma.
- Manage superficial basal cell carcinoma, particularly when surgery is not an option.
- Clear HPV-related skin lesions, such as genital or perianal warts.
- Provide a non-surgical, field-directed therapy for areas with multiple lesions.
→ Additional benefits include:
- Improving skin health by treating subclinical (hidden) lesions.
- Offering a home-based treatment option under medical supervision.
- Reducing the need for multiple cryotherapy or surgical procedures.
Alternatives
→ Alternatives to imiquimod cream include:
- Topical 5-FU (5-fluorouracil) → another field therapy option targeting sun-damaged skin.
- Diclofenac gel → anti-inflammatory topical treatment, milder and slower-acting.
- Ingenol mebutate gel → less common now due to safety concerns.
- Cryotherapy → freezing lesions individually with liquid nitrogen.
- Photodynamic therapy (PDT) → light-based destruction of abnormal cells after applying a photosensitizer.
- Laser therapy or chemical peels → improve skin appearance while treating precancerous lesions.
→ Dermatologists may alternate or combine these therapies based on severity, skin type, and tolerance.
Preparation
→ Before starting imiquimod cream, patients should:
- Consult a dermatologist → to confirm diagnosis and suitability for treatment.
- Identify treatment area → face, scalp, trunk, or genital region.
- Avoid sunburn or tanning → inflamed or sunburned skin reacts more strongly.
- Stop harsh skincare → discontinue strong exfoliants or retinoids 3–5 days before therapy.
- Plan downtime → since redness, peeling, and scabbing may occur, patients may want to schedule around work or social events.
- Baseline photos → often taken to document starting condition for progress monitoring.
How it’s Done
→ An Imiquimod cream plan typically follows these steps:
- Application → cream is applied to the treatment area, usually 2–5 times per week, depending on condition and prescription.
- Duration → treatment lasts 2–6 weeks for actinic keratoses; 6–16 weeks for basal cell carcinoma or warts.
- Reaction phase → redness, irritation, scabbing, and peeling appear as the immune system attacks abnormal cells.
- Monitoring → dermatologists may adjust frequency if irritation is excessive.
- Completion → treatment is stopped after the prescribed course, followed by a healing period.
- Follow-up → dermatologist checks whether lesions are fully cleared and decides if additional cycles are needed.
Recovery
→ Recovery depends on the treatment site and duration:
- During treatment → redness, scaling, itching, and discomfort are common.
- Post-treatment healing → skin usually recovers within 2–4 weeks after stopping therapy.
- Appearance → initially, the treated area may look worse before it improves, as lesions crust and fall off.
- Skin improvements → smoother texture, clearer tone, and reduction of precancerous lesions are typically visible after recovery.
→ Patients should:
- Use gentle cleansers and moisturizers.
- Avoid direct sunlight and use broad-spectrum sunscreen daily.
- Follow dermatologist’s post-care instructions strictly.
Complications
→ Common temporary side effects include:
- Redness, swelling, and irritation.
- Itching, burning, or pain at the application site.
- Crusting, scabbing, or oozing.
- Flu-like symptoms (rare but possible).
→ Rare complications:
- Persistent pigmentation changes (lighter or darker spots).
- Severe allergic reactions.
- Scarring (uncommon, usually after prolonged misuse).
→ Side effects are generally temporary and resolve after treatment stops. Proper medical supervision greatly reduces risks.
Treatment options in Korea
→ Korea offers advanced dermatology care and structured imiquimod cream plans, especially for sun damage, precancerous lesions, and skin cancers.
- University hospitals such as Seoul National University Hospital, Asan Medical Center, and Samsung Medical Center provide specialized protocols for imiquimod use.
- Customized dosing schedules → dermatologists adjust application frequency based on patient skin sensitivity.
- Combination therapy → often paired with cryotherapy, PDT, or laser treatments for better clearance.
- Follow-up care → Korean clinics emphasize regular monitoring, digital photography, and mole mapping to track results.
- Cosmetic integration → dermatologists often combine imiquimod therapy with rejuvenating treatments (like chemical peels or gentle lasers) after healing.
- Preventive education → strict guidance on sunscreen use, UV avoidance, and lifestyle adjustments is a key part of Korean dermatology plans.
- Medical tourism support → international patients can access imiquimod plans in Korea with English-speaking specialists and advanced dermatology clinics.
→ With its combination of clinical precision, modern technology, and preventive focus, Korea provides highly effective and patient-friendly imiquimod cream treatment plans.