What it is
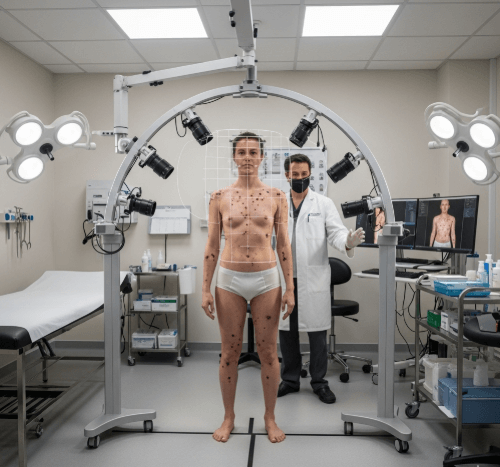
→ Full body mole mapping is a specialized dermatological procedure that creates a detailed photographic record of all moles and pigmented lesions on a patient’s skin.
→ High-resolution images are taken of the entire body and stored digitally. These serve as a baseline reference so dermatologists can compare and track changes in moles over time.
→ The process is especially important for detecting skin cancer early, including melanoma, which often develops from a changing mole.
→ Mole mapping is recommended for individuals at high risk of skin cancer or those with many atypical moles. It allows dermatologists to notice even subtle changes that might otherwise go undetected during regular skin checks.
Why it’s done
→ The main reason for mole mapping is early cancer detection.
→ Benefits include:
- Detecting new or evolving moles before they become malignant.
- Differentiating between stable moles and suspicious ones that require biopsy.
- Reducing unnecessary biopsies by comparing images over time.
- Providing peace of mind to patients with many moles or a family history of melanoma.
- Helping dermatologists establish a long-term skin health record for accurate follow-up.
→ For patients with fair skin, frequent sun exposure, or genetic risk factors, full body mole mapping can be life-saving.
Alternatives
→ Alternatives to full body mole mapping include:
- Standard skin screening exam → dermatologist visually inspects moles without a photographic baseline.
- Self-examination → patients monitor moles at home using mirrors or smartphone photos.
- Mobile mole apps → AI-based apps that analyze photos for suspicious moles, though accuracy varies.
→ These alternatives can be useful, but they lack the precision and reliability of professional mole mapping with high-resolution imaging.
Preparation
→ Preparing for mole mapping ensures accurate results:
- Avoid tanning → sunburn or tanning can temporarily change mole appearance, making results unreliable.
- No makeup or nail polish → skin must be fully visible.
- Wear minimal clothing → patients are usually asked to change into a medical gown.
- List medical history → provide details about past skin cancers, family history, and mole removals.
- Previous records → bring old photos or pathology reports if available.
- Hair management → excessive body hair may sometimes be trimmed in specific areas for better imaging.
How it’s Done
→ The process is painless and typically follows these steps:
- Initial consultation → dermatologist reviews medical history and risk factors.
- High-resolution photography → multiple digital images are taken of the entire body, including scalp, face, back, chest, arms, legs, hands, feet, and hidden areas.
- Dermoscopy integration → close-up dermoscopic photos are taken of atypical or suspicious moles.
- Image storage → all images are securely stored in digital archives for future comparison.
- Analysis and discussion → dermatologist reviews results with the patient and explains which moles to monitor.
- Follow-up plan → repeat mapping is recommended every 6–12 months depending on risk level.
→ The session usually takes 30–60 minutes, depending on the number of moles.
Recovery
→ Mole mapping is a non-invasive procedure and requires no recovery time.
→ Patients can return to normal activities immediately.
→ If a mole appears suspicious during mapping and a biopsy is performed, recovery involves:
- Mild soreness for 1–3 days.
- Simple wound care with ointment and a bandage.
- Healing within 1–2 weeks.
→ Regular follow-up mapping sessions allow long-term tracking without risk or downtime.
Complications
→ Full body mole mapping itself carries no complications since it is non-invasive.
→ Possible risks come only if a biopsy is performed:
- Minor pain or bleeding.
- Temporary scarring.
- Low infection risk if aftercare is not followed.
→ The greatest danger is not undergoing mole mapping in high-risk patients, since melanoma can progress unnoticed without accurate monitoring.
Treatment options in Korea
→ Korea is a leader in advanced dermatology and preventive care, making mole mapping widely accessible.
- High-tech clinics in Seoul, Busan, and Daegu offer state-of-the-art digital mole mapping with dermoscopy integration.
- AI-assisted analysis → many Korean clinics use artificial intelligence to detect suspicious mole changes.
- International standards → hospitals like Seoul National University Hospital and Samsung Medical Center follow global guidelines for melanoma detection.
- Frequent follow-ups → Korean dermatology emphasizes preventive care, encouraging patients to return every 6–12 months for new image updates.
- Integration with cosmetic care → dermatologists often combine mole mapping with skin rejuvenation advice and sun protection regimens.
- Expat-friendly services → due to Korea’s reputation as a medical tourism hub, many clinics offer English-language consultations for international patients.
→ With its combination of cutting-edge imaging technology, skilled dermatologists, and preventive focus, Korea provides some of the most reliable full body mole mapping services worldwide.