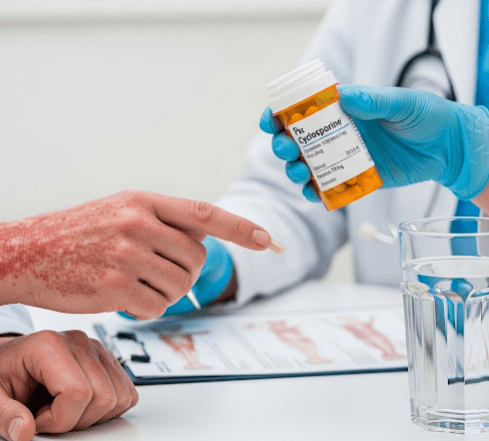
What it is
➝ Cyclosporine is an immunosuppressive medication originally developed for organ transplant patients to prevent rejection. In dermatology, it is used as a rescue therapy for severe, rapidly worsening psoriasis.
➝ The term “rescue” means cyclosporine is often prescribed for short-term, urgent control when psoriasis flares are extensive, disabling, or unresponsive to other treatments.
➝ It works by suppressing T-cell activity, which plays a major role in the immune system’s overreaction that drives psoriasis. By reducing this activity, cyclosporine quickly decreases inflammation, redness, and scaling.
➝ Unlike topical agents, cyclosporine acts systemically and is reserved for moderate-to-severe plaque psoriasis, erythrodermic psoriasis, and pustular psoriasis.
Why it’s done
→ To rapidly control severe flare-ups of psoriasis that threaten a patient’s health or quality of life.
→ To stabilize erythrodermic or pustular psoriasis, which can be dangerous and sometimes life-threatening.
→ To provide a short-term bridge therapy while transitioning patients to safer, long-term options like methotrexate, acitretin, or biologics.
→ To help patients who failed or cannot tolerate other systemic drugs.
→ In Korea, cyclosporine is used strategically in hospital-based dermatology clinics, where monitoring and rapid intervention are possible.
Alternatives
→ Methotrexate: Effective for chronic, moderate-to-severe psoriasis and psoriatic arthritis.
→ Acitretin: An oral retinoid often used in combination with phototherapy for resistant psoriasis.
→ Phototherapy: Narrowband UVB or PUVA therapy for less aggressive cases.
→ Biologics: Highly targeted injections (e.g., IL-17, IL-23, TNF-alpha blockers) that are often chosen for long-term management.
→ Systemic corticosteroids: Rarely used due to rebound risks, but sometimes given in hospital emergencies.
Preparation
→ Before starting cyclosporine, patients undergo baseline testing:
- Kidney function (serum creatinine, BUN)
- Liver function tests
- Blood pressure measurement
- Lipid panel and blood sugar levels
→ Patients are screened for hypertension, kidney disease, or history of cancer, as cyclosporine can worsen these conditions.
→ Drug interactions must be carefully reviewed since cyclosporine interacts with many common medications.
→ Patients are advised to avoid grapefruit juice, which can dangerously increase drug levels.
→ In Korea, dermatologists provide structured pre-treatment counseling to explain risks and the temporary nature of cyclosporine therapy.
How it’s Done
→ Cyclosporine is taken orally in capsule form.
→ The dose is usually calculated based on body weight (2.5–5 mg/kg per day).
→ It is typically prescribed for short-term use (up to 12–16 weeks) to control severe flares.
→ Once improvement occurs, the dose is gradually tapered, and patients are transitioned to safer long-term treatments.
→ Regular monitoring of blood pressure and kidney function is mandatory, often every 2–4 weeks.
→ In Korea, clinics often combine cyclosporine with topical moisturizers, tar-based shampoos, and supportive skin care for comfort.
Recovery
→ Improvement is often seen within 2–4 weeks, which makes cyclosporine one of the fastest-acting systemic treatments for psoriasis.
→ Skin plaques typically shrink, redness subsides, and itching reduces dramatically.
→ Patients often report better sleep, improved mobility, and reduced psychological stress once their symptoms are under control.
→ Recovery is monitored closely to avoid side effects, and treatment is stopped once stability is achieved.
→ After discontinuation, psoriasis often returns, so transition therapy is essential.
Complications
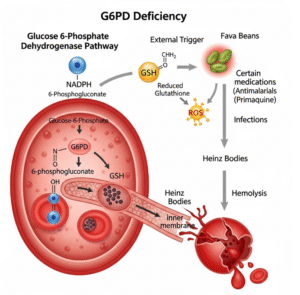
→ Common short-term effects: Headache, nausea, increased hair growth, and gum swelling.
→ Serious risks:
- Nephrotoxicity (kidney damage), especially with prolonged use.
- Hypertension, which can lead to cardiovascular problems.
- Increased risk of infections due to immune suppression.
- Increased cancer risk (particularly skin cancer and lymphoma) if used long term.
→ Because of these risks, cyclosporine is not suitable for continuous use in psoriasis patients.
→ Patients must strictly adhere to monitoring schedules and lifestyle advice to reduce complications.
Treatment Options in Korea
→ Korean dermatology centers often use cyclosporine as a short-term rescue therapy in patients hospitalized for severe psoriasis flares.
→ It is usually integrated into a stepwise approach: cyclosporine for quick control, followed by a switch to methotrexate or biologics for long-term management.
→ Korean clinics emphasize individualized dosing and use advanced monitoring systems to track blood pressure and kidney health.
→ Many hospitals offer combination regimens where cyclosporine is paired with phototherapy or topical therapy to reduce drug dose and side effects.
→ Patients receive comprehensive aftercare programs, including dietary counseling (low salt, kidney-friendly diets), psychological support, and follow-up visits.
→ In Korea, cyclosporine is regarded as a life-saving tool for aggressive psoriasis, but doctors are careful to avoid long-term risks by switching patients to safer therapies as soon as possible.