What it is
➝ Contact dermatitis is an inflammatory skin condition triggered by allergen or irritant exposure, leading to redness, itching, swelling, and scaling.
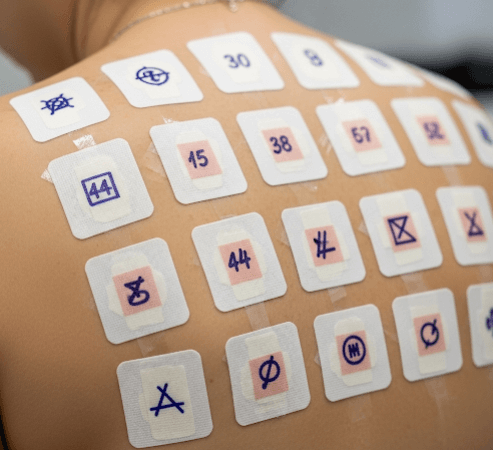
➝ When allergic contact dermatitis is suspected, patch testing is the gold standard diagnostic tool.
➝ Patch testing involves applying small amounts of common allergens under occlusion on the patient’s back for 48 hours, followed by evaluation of skin reactions.
➝ In Korea, patch testing is widely performed in dermatology and allergy clinics using standardized allergen panels tailored to Korean environmental and occupational exposures.
Why it’s done
→ To identify the specific allergen(s) responsible for dermatitis.
→ To guide allergen avoidance, reducing flare-ups and dependence on corticosteroids.
→ To differentiate between irritant contact dermatitis, allergic contact dermatitis, and atopic eczema overlap.
→ To improve long-term outcomes by enabling patients to adjust personal care products, workplace habits, and lifestyle.
→ In Korea, patch testing is especially important for patients with chronic hand eczema, facial dermatitis, or occupational skin disease.
Alternatives
→ Clinical history alone: May suggest allergens but often inaccurate.
→ Skin prick testing: Used for immediate-type allergies (e.g., pollen, food), not delayed-type like contact dermatitis.
→ Repeat open application test (ROAT): Applying product on forearm daily for 1–2 weeks, useful for cosmetics but less standardized.
→ Elimination and re-exposure: Avoiding suspected allergens and observing improvement, but not precise.
Preparation
→ Patient should stop topical steroids and immunosuppressants on the test area for at least 1 week before testing.
→ Oral corticosteroids and systemic immunosuppressants should be avoided if possible, as they can suppress test results.
→ The back should be free of eczema, infection, or sunburn.
→ In Korea, dermatologists often screen patient history to choose additional allergens relevant to occupation or cosmetic use.
How it’s Done
→ Day 1 (Application):
- Allergens are applied in small aluminum or plastic chambers (Finn Chambers) on adhesive tape.
- Common panels include nickel, cobalt, fragrance mix, preservatives (formaldehyde, parabens, isothiazolinone), rubber chemicals, hair dye (PPD), and local allergens such as certain herbal extracts or K-beauty product ingredients.
- Patches are left on for 48 hours.
→ Day 3 (First reading):
- Patches are removed.
- Dermatologist inspects sites for redness, swelling, papules, or vesicles.
→ Day 5–7 (Second reading):
- Delayed reactions are checked, as some allergens (neomycin, corticosteroids, fragrance) react late.
→ Results are graded (negative, doubtful, +, ++, +++) according to international guidelines.
→ In Korea, patients often receive a personalized allergen avoidance list with both chemical names and consumer product alternatives.
Recovery
→ Testing itself may cause mild itching or redness at positive sites, which usually resolves within a few days.
→ Patients gain long-term benefit by avoiding identified allergens, often leading to significant improvement in chronic dermatitis.
→ Education on safe substitutes for personal care and household items enhances recovery.
Complications
→ Irritant reactions: Non-allergic redness from test chambers or adhesives.
→ Angry back syndrome: Multiple false positives due to highly reactive skin.
→ Persistent pigmentation or rarely scarring at strong positive sites.
→ Flare-up of eczema in active dermatitis patients.
→ With correct technique and patient preparation, patch testing is safe and effective.
Treatment Options in Korea
→ Korean dermatology clinics use both international standard allergen panels and Korean-specific series, which include common allergens in cosmetics, hair dyes, rubber gloves, adhesives, and occupational exposures.
→ The Korean Contact Dermatitis Research Group (KCDRG) has developed standardized patch test series adapted to the Korean population.
→ Many clinics supplement with cosmetic and personal care products brought by patients, testing for reactions to real-life items.
→ After results, patients are given printed allergen avoidance lists, including alternative K-beauty and household products safe for use.
→ Education is emphasized: dermatologists explain how to read ingredient labels and avoid hidden allergens.
→ With Korea’s structured system, patch testing not only diagnoses the cause but also leads to personalized, practical care plans that improve long-term outcomes in contact dermatitis.