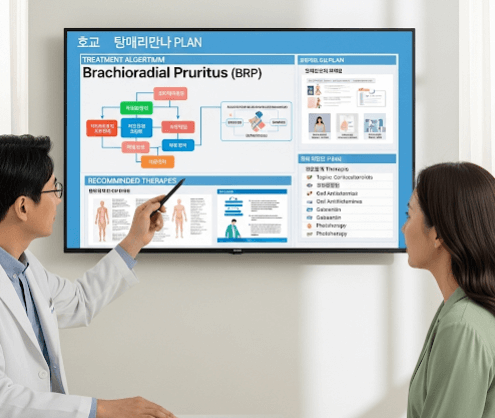
What it is
➝ Brachioradial pruritus (BRP) is a chronic neuropathic itch syndrome that affects the dorsolateral forearms, sometimes extending to the upper arms or shoulders.
➝ Patients describe intense itching, tingling, burning, or stinging without a primary rash, although secondary excoriations, lichenification, or hyperpigmentation may develop from scratching.
➝ The cause is thought to be a mix of cervical spine pathology (nerve compression at C5–C8) and chronic sun exposure, which sensitizes cutaneous nerves.
➝ In Korea, management of BRP is multidisciplinary, involving dermatology, neurology, and rehabilitation medicine.
Why it’s done
→ To relieve chronic itch and neuropathic sensations that interfere with sleep and daily life.
→ To prevent secondary skin changes like scarring or pigmentation.
→ To address underlying musculoskeletal or cervical spine factors.
→ To restore quality of life, since untreated BRP can persist for months or years.
Alternatives / Treatment Options
General measures
→ Avoid UV exposure, heat, and activities that extend the neck.
→ Use cool compresses or menthol/pramoxine lotions for temporary relief.
→ In Korea, UV-protective sleeves and sunscreen are often recommended.
Topical therapy
→ Capsaicin cream or patches to desensitize nerve endings.
→ Topical anesthetics (lidocaine creams or patches).
→ Corticosteroids only if secondary eczema is present.
→ Specialty pharmacies in Korea sometimes prepare compounded capsaicin-lidocaine creams.
Systemic therapy
→ Gabapentin or pregabalin as first-line neuropathic agents.
→ Tricyclic antidepressants (amitriptyline, doxepin) or mirtazapine for itch with insomnia.
→ SSRIs or SNRIs in cases with anxiety or depression.
→ Antihistamines mainly for sedation, since histamine is not the main mediator.
Procedural / advanced therapy
→ Cervical physiotherapy: posture correction, traction, strengthening.
→ MRI imaging to rule out disc herniation or spondylosis if indicated.
→ Botulinum toxin injections for refractory cases.
→ Nerve blocks in severe, resistant itch.
→ Phototherapy (NB-UVB) in selected diffuse neuropathic itch.
Preparation
→ Careful history and exam to confirm localized neuropathic itch.
→ Rule out dermatologic mimics like eczema or psoriasis.
→ Cervical spine evaluation if neurological symptoms are present.
→ In Korea, collaboration between dermatologists and rehabilitation specialists is common.
How it’s Done
→ Step 1: Begin with general measures (UV avoidance, cooling, emollients) and topical therapy.
→ Step 2: Escalate to systemic neuropathic agents (gabapentin, pregabalin, TCAs).
→ Step 3: Add physiotherapy or posture correction if cervical disease is suspected.
→ Step 4: Consider advanced interventions (botulinum toxin, nerve block) for refractory cases.
→ Step 5: Maintain long-term management with UV protection, posture care, and medications as needed.
Recovery
→ Partial relief is common within 2–4 weeks of neuropathic medication.
→ Capsaicin may help daily itching but requires consistent use.
→ Physiotherapy improves symptoms over weeks to months when cervical contribution is significant.
→ Many patients need chronic, combined management to maintain control.
Complications
→ Persistent itch with risk of lichenification and pigmentation.
→ Side effects of systemic therapy: sedation, dizziness, dry mouth, constipation.
→ Irritation from topical capsaicin or lidocaine if overused.
→ Psychological distress from chronic symptoms.
Treatment Options in Korea
→ Dermatology clinics often start with capsaicin cream and gabapentin or pregabalin.
→ Rehabilitation medicine provides posture correction and cervical therapy.
→ Advanced centers in Seoul and Busan use botulinum toxin and nerve block techniques for refractory cases.
→ Phototherapy is available in major hospitals for patients with widespread neuropathic itch.
→ Korean patients are counseled extensively on UV protection, posture habits, and lifestyle modifications to prevent recurrence.