What It Is
Free flap reconstruction is an advanced surgical procedure where tissue from one part of the body (skin, fat, muscle, or bone) is transplanted to another area, along with its blood vessels. Using microsurgery, the surgeon reconnects the flap’s blood vessels to those at the recipient site to ensure proper blood flow and long-term survival of the transplanted tissue.
In Korea, this surgery is widely performed in specialized plastic and reconstructive surgery centers. Korean surgeons are known for their expertise in supermicrosurgery, 3D planning, and aesthetic refinement, which are especially important for both function and appearance in reconstructive procedures.
Why It’s Done
Free flap reconstruction is used when simpler methods (like skin grafts or local flaps) cannot provide sufficient tissue or function. It is typically done for:
- Head and neck cancer reconstruction (jaw, tongue, pharynx, or face after tumor removal).
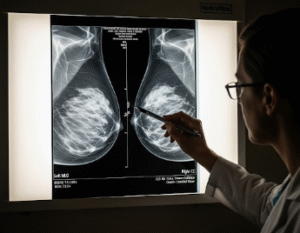
- Breast reconstruction after mastectomy.
- Trauma repair following severe accidents or burns.
- Bone reconstruction (e.g., using fibula bone for jaw repair).
- Chronic wounds or infections that do not heal with conventional methods.
The purpose is not only cosmetic improvement but also to restore essential functions such as eating, speaking, swallowing, or walking.
Alternatives
Other treatment options may include:
- Skin grafting: Suitable for small, superficial defects but limited for deep or complex wounds.
- Local or regional flaps: Moving tissue from an area near the defect while maintaining its blood supply.
- Artificial or bioengineered substitutes: Used for temporary coverage but not for large or complex defects.
- Prosthetics: Sometimes chosen instead of surgical reconstruction, especially after cancer removal.
Free flap surgery is considered when the defect is too large or functionally important for simpler solutions.
Preparation
Preparation before surgery usually involves:
- Consultation: Evaluation of the defect, possible donor sites, and functional needs.
- Imaging: CT angiography or Doppler studies to assess blood vessels at both donor and recipient sites.
- Medical clearance: Blood tests, anesthesia evaluation, and general health assessment.
- Lifestyle adjustments: Stopping smoking and alcohol at least 4 weeks before surgery to promote healing.
- Patient education: Discussion of possible donor site effects, recovery time, and rehabilitation needs.
How It’s Done
Free flap reconstruction is performed under general anesthesia and can last 6–12 hours depending on complexity. Steps include:
- Donor site harvest: Skin, fat, muscle, or bone is carefully removed along with its artery and vein.
- Recipient site preparation: The defect area is prepared to receive the new tissue.
- Microsurgical connection: Blood vessels of the flap (often just 1–3 mm wide) are reconnected to local vessels under a microscope.
- Shaping: The flap is molded to restore natural contour and function.
- Closure: Both donor and recipient sites are closed; skin grafts may be used at the donor site if needed.
Recovery
Recovery after free flap surgery is more intensive than standard reconstructive procedures:
- Hospital stay: Usually 1–2 weeks to closely monitor flap survival.
- First days: Nurses and surgeons frequently check blood flow to the flap.
- Mobility: Early walking is encouraged, but donor site activity may be restricted.
- Rehabilitation: Physical therapy, speech therapy, or swallowing therapy may be required depending on reconstruction site.
- Long-term recovery: Initial healing occurs in 4–6 weeks; final functional and cosmetic results may take 6–12 months.
Possible Complications
Like any major surgery, free flap reconstruction carries some risks:
- Flap failure due to blood vessel clotting.
- Infection or delayed wound healing.
- Donor site complications (weakness, scarring, or numbness).
- Contour irregularities or asymmetry.
- Blood clots or deep vein thrombosis (DVT).
- Rare anesthesia-related risks.
Korea’s specialized microsurgical teams help minimize these risks with advanced monitoring and techniques.
Treatment Options in Korea
Diagnosis
- 3D imaging and CT angiography for surgical planning.
- Multidisciplinary evaluation (oncology, reconstructive surgery, rehabilitation).
Medical Treatments
- Pain control, antibiotics, and anticoagulants after surgery.
- Wound care and scar management for both donor and recipient sites.
Surgical or Advanced Therapies
- Cutaneous or fasciocutaneous flaps: For skin and soft tissue coverage.
- Musculocutaneous flaps: Combining muscle and skin for durability.
- Osseous flaps (e.g., fibula flap): For bone reconstruction of the jaw, face, or limbs.
- Perforator flaps: Preserving donor site muscle while transferring only skin and fat.
- Combined approaches: With dental implants, prosthetics, or other reconstructive methods.
Rehabilitation and Support
- Physiotherapy to restore movement and strength.
- Speech/swallowing therapy for head and neck cases.
- Long-term follow-up for scar care and functional monitoring.
- International patient support including interpreters, care coordinators, and virtual follow-ups.