What It Is
Facial nerve reanimation is a surgical procedure that restores movement and expression to the face after facial paralysis caused by trauma, tumor removal, infection, or congenital conditions like Moebius syndrome. Facial paralysis not only affects appearance but also interferes with speech, eating, blinking, and emotional expression.
Reanimation involves different approaches such as nerve grafts, nerve transfers, muscle transfers, or cross-facial nerve grafts. In Korea, surgeons use microsurgery, high-definition imaging, and nerve monitoring to achieve both functional recovery and natural aesthetic results.
Why It’s Done
Patients undergo facial nerve reanimation because:
- They cannot move parts of their face due to nerve damage.
- They experience difficulty with eye closure, smiling, eating, or speech.
- Asymmetry impacts self-esteem and social interactions.
- Conservative treatments have failed to restore meaningful movement.
Good candidates include:
- Patients with long-standing or complete facial paralysis.
- Individuals in good general health, able to undergo microsurgery.
- Children or adults with congenital or acquired paralysis seeking functional and cosmetic recovery.
Alternatives
- Physical therapy and facial retraining: Helpful for mild paralysis.
- Botulinum toxin injections: Can reduce asymmetry by weakening overactive muscles.
- Static procedures (slings or grafts): Provide symmetry at rest but not active movement.
Preparation
Before surgery in Korea, patients will:
- Have a neurological and functional exam, including smile and eye closure assessment.
- Undergo imaging (MRI or CT) to evaluate facial nerve integrity.
- Receive EMG studies to check remaining nerve activity.
- Stop smoking and alcohol at least 4 weeks before surgery.
- Prepare for staged procedures and long rehabilitation if needed.
How It’s Done
- Anesthesia: General anesthesia is required.
- Techniques vary depending on severity:
- Nerve grafting: Bridges gaps in damaged facial nerves using donor nerves.
- Nerve transfers: Redirects nearby nerves (e.g., hypoglossal or masseter nerve) to restore facial function.
- Cross-facial nerve graft (CFNG): Uses sural nerve graft to bring impulses from the healthy side of the face.
- Free functional muscle transfer: Transplants muscles such as the gracilis (from the thigh) to restore smiling ability.
- Duration: 4–12 hours depending on the technique.
Recovery
- First week: Swelling, bruising, and mild pain are common.
- Hospital stay: 5–10 days depending on complexity.
- Nerve regeneration: Recovery is gradual, as nerves grow slowly (about 1 mm per day).
- Physical therapy: Essential for retraining new muscle movements.
- Final results: Visible improvement may take 6–18 months, with gradual return of facial function and expression.
Possible Complications
- Partial recovery or incomplete facial movement.
- Donor site morbidity (numbness, weakness, or scarring where nerve or muscle was taken).
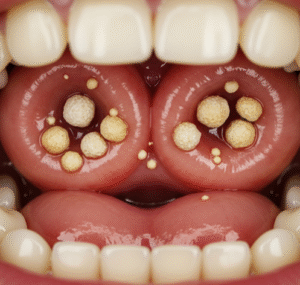
- Synkinesis (involuntary movement when trying to move another muscle).
- Infection, wound healing issues, or vascular complications in free flap transfers.
Treatment Options in Korea
Diagnosis
Korean surgeons use EMG, nerve conduction studies, MRI, and 3D facial imaging to evaluate the extent of paralysis and design customized treatment plans.
Medical Treatments
- Physiotherapy and retraining for mild cases.
- Botox or filler injections to improve symmetry.
Surgical or Advanced Therapies
- Nerve grafts and transfers (hypoglossal or masseter to facial nerve).
- Cross-facial nerve grafts (CFNG) for bilateral coordination.
- Free functional muscle transfer (gracilis muscle) to restore dynamic smiling.
- Combination procedures for complex or long-standing paralysis.
Rehabilitation and Support
- Structured facial physiotherapy programs to optimize results.
- Scar management with silicone gels or laser treatments.
- Long-term follow-ups with nerve testing to monitor regeneration.
- International patients benefit from Korea’s microsurgical expertise, multidisciplinary teams, and multilingual rehabilitation support.