What it is
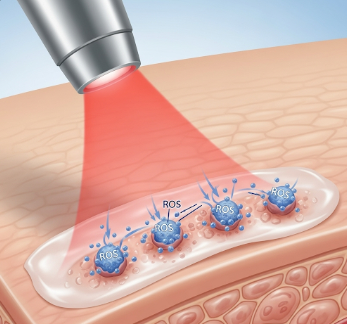
Photodynamic Therapy (PDT) is a minimally invasive medical treatment that uses a combination of light-sensitive drugs (photosensitizers) and a specific wavelength of light to destroy abnormal or diseased cells. PDT is primarily used to treat certain cancers, precancerous conditions, and skin disorders.
➡ How it works:
- A photosensitizing agent is applied to the affected area or administered intravenously.
- The agent is absorbed preferentially by abnormal cells.
- When exposed to a specific light source, the drug becomes activated, producing reactive oxygen species that selectively destroy targeted cells.
💡 Key points:
- PDT is targeted, minimizing damage to surrounding healthy tissue.
- Often combined with other therapies for better treatment outcomes.
- In Korea, PDT is offered in specialized dermatology and oncology centers, using advanced equipment and strict safety protocols.
Why it’s done
Photodynamic therapy is used for therapeutic and cosmetic purposes, particularly where precision and minimal invasiveness are essential.
➤ Medical indications include:
- Skin cancers → Basal cell carcinoma, squamous cell carcinoma, actinic keratosis
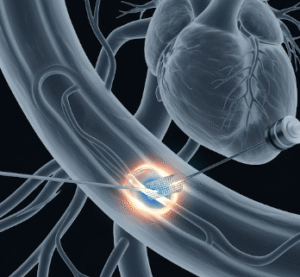
- Certain internal cancers → Esophageal, lung, bladder cancers (early-stage or localized)
- Precancerous conditions → Barrett’s esophagus or dysplastic lesions
- Acne and dermatologic disorders → Severe acne, photoaging, or rosacea in dermatology
- Macular degeneration → PDT can reduce abnormal blood vessel growth in the eye
➤ Key benefits:
- Selective targeting reduces damage to healthy tissues
- Minimally invasive with reduced recovery time
- Repeatable treatment if necessary
- Can be combined with surgery, chemotherapy, or radiotherapy for enhanced results
- Provides cosmetic benefits in skin treatments by reducing scarring
Alternatives
While PDT is highly effective in selected cases, alternatives may include:
✔ Surgical excision → Removal of cancerous or precancerous tissue
✔ Cryotherapy → Freezing abnormal cells with extreme cold
✔ Radiation therapy → Uses high-energy rays to destroy cancer cells
✔ Topical chemotherapy → Creams like 5-fluorouracil for precancerous lesions
✔ Laser therapy → Ablation of skin lesions or vascular anomalies
Note: The choice between PDT and alternatives depends on lesion type, size, location, patient health, and cosmetic considerations. PDT is often preferred for superficial or localized lesions where tissue preservation is important.
Preparation
Proper preparation ensures optimal outcomes and safety during PDT:
🔹 Medical evaluation
- Comprehensive examination of the lesion(s) and medical history
- Laboratory tests if PDT involves systemic photosensitizers
🔹 Medication and lifestyle guidance
- Avoid photosensitizing medications unless instructed by the doctor
- Limit sun exposure before and after treatment to prevent unintended reactions
🔹 Skin and lesion preparation
- Clean the treatment area thoroughly
- Shave or debride lesions if recommended for better photosensitizer absorption
🔹 Patient education
- Discuss expected outcomes, potential side effects, and post-treatment care
- Schedule follow-up visits for monitoring response and additional sessions
How it’s done
PDT involves two main components: application of a photosensitizer and light activation.
➡ Step-by-step procedure:
- Photosensitizer application
- Topical: Cream applied directly to skin lesions
- Intravenous: Administered for internal cancers
- Incubation period: Allows absorption into abnormal cells (typically 1–3 hours for skin lesions, longer for internal tumors)
- Light activation
- Specific wavelength of light (laser, LED, or other devices) is directed at the lesion
- Light activates the photosensitizer, producing reactive oxygen species
- Causes selective cell death while sparing healthy tissue
- Post-procedure care
- Area may be cooled or treated with topical agents to reduce discomfort
- Dressings applied if necessary
- Instructions given for sun avoidance to prevent photosensitivity reactions
⏱ Procedure duration: Usually 30–90 minutes depending on lesion size and location
💡 Tips for accuracy and safety:
- Patients must follow light exposure restrictions after systemic photosensitizers
- Multiple sessions may be required for complete lesion resolution
Recovery / Expected Outcomes
Recovery from PDT is generally quick, especially for skin treatments:
🔹 Skin treatment recovery:
- Mild redness, swelling, or crusting may occur for several days
- Healing time: 1–2 weeks, depending on lesion size
- Minimal scarring compared to surgical excision
🔹 Internal tumor treatment recovery:
- Patients may experience temporary discomfort, nausea, or localized inflammation
- Recovery time is usually shorter than conventional surgery
- Follow-up imaging or endoscopy may be performed to assess treatment response
🔹 Clinical outcomes:
- High lesion clearance rates for superficial cancers and precancerous conditions
- Repeated sessions can achieve optimal results without significant tissue damage
- Combined therapy may enhance long-term survival in internal cancers
Complications / Considerations
Although PDT is generally safe, some risks and considerations include:
⚠ Photosensitivity reactions → Patients must avoid direct sunlight for 24–48 hours (topical) or up to several weeks (systemic)
⚠ Local skin reactions → Redness, swelling, itching, blistering, or crusting
⚠ Pain or discomfort → During or immediately after light activation
⚠ Incomplete treatment → Some lesions may require additional sessions
⚠ Rare systemic reactions → Allergic reactions to photosensitizers or temporary nausea
Mitigation:
- Strict adherence to light avoidance instructions
- Pre- and post-procedure counseling by trained medical staff
- Proper selection of patients based on lesion type, size, and overall health
Treatment Options in Korea
PDT is widely available in Korea, particularly in dermatology, oncology, and ophthalmology centers, with modern equipment and specialized care teams:
🏥 Hospitals and clinics offering PDT:
- Seoul National University Hospital (SNUH) → Comprehensive PDT services for skin, internal cancers, and ocular conditions
- Asan Medical Center → Advanced PDT with lasers, LED systems, and combination therapy options
- Samsung Medical Center → Minimally invasive PDT for precancerous lesions and early-stage cancers
- Specialized dermatology clinics → PDT for acne, photoaging, and vascular lesions
💰 Insurance and cost:
- National Health Insurance covers certain indications, especially precancerous lesions and early-stage cancers
- Private insurance may cover cosmetic PDT treatments or specialized tumor therapy
- Costs vary depending on lesion type, treatment complexity, and number of sessions
🔹 Additional support:
- Pre- and post-procedure counseling on photosensitivity precautions
- Follow-up sessions to monitor healing and treatment efficacy
- Integration with other therapies such as surgery, chemotherapy, or laser therapy
Conclusion
Photodynamic Therapy (PDT) in Korea is a safe, effective, and minimally invasive treatment for a variety of conditions, including skin cancers, internal tumors, precancerous lesions, and dermatologic disorders.
By combining targeted photosensitizers and light activation, PDT offers:
- Selective destruction of abnormal cells
- Minimized damage to healthy tissue
- Rapid recovery and reduced scarring
- Flexibility to be combined with other treatments for enhanced results