What it is
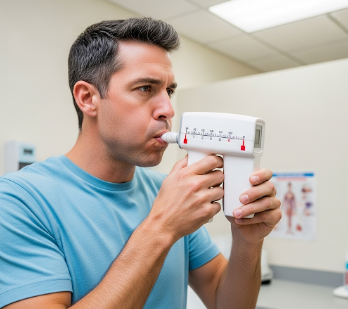
A peak flow test is a simple, non-invasive procedure used to measure how well air moves out of the lungs, specifically assessing the peak expiratory flow (PEF). This measurement helps monitor lung function, particularly in people with asthma or other respiratory conditions.
➡ Purpose of the test:
- Evaluate airway obstruction
- Track changes in lung function over time
- Detect early signs of worsening asthma or respiratory disease
💡 Key points:
- The test is performed using a peak flow meter, a small, handheld device.
- Results are recorded in liters per minute (L/min) and compared to predicted normal values based on age, sex, and height.
- It can be conducted at home or in a clinical setting.
In Korea, peak flow testing is a common component of asthma management programs, with doctors, nurses, and respiratory therapists guiding patients on proper technique and interpretation of results.
Why it’s done
Peak flow tests are essential for monitoring respiratory health and preventing complications.
➤ Medical indications include:
- Asthma → Regular monitoring to detect flare-ups or worsening symptoms
- Chronic obstructive pulmonary disease (COPD) → Helps track disease progression
- Exercise-induced bronchoconstriction → Evaluates lung function during physical activity
- Respiratory infections → Detects temporary reduction in airflow
➤ Key benefits:
- Early detection of airway constriction before symptoms worsen
- Helps guide treatment adjustments, including medication changes
- Empowers patients to take active control of their respiratory health
- Improves safety by preventing severe asthma attacks or breathing crises
Alternatives
While the peak flow test is convenient, other assessments may complement or replace it:
✔ Spirometry → Measures forced expiratory volume and other detailed lung function parameters
✔ Pulse oximetry → Monitors blood oxygen levels
✔ Bronchial challenge tests → Evaluate airway hyperresponsiveness
✔ Clinical symptom tracking → Diary of coughing, wheezing, and shortness of breath
✔ Exhaled nitric oxide testing → Assesses airway inflammation
Note: Peak flow testing is particularly effective for daily self-monitoring due to its simplicity and portability, whereas alternatives are often more comprehensive and performed in clinical settings.
Preparation
Before performing a peak flow test, proper preparation ensures accurate results:
🔹 Choose the right device
- Use a calibrated peak flow meter
- Ensure the device is clean and free of obstructions
🔹 Patient preparation
- Stand up straight for the best lung expansion
- Avoid heavy meals or smoking immediately before the test
- Remove dentures if they interfere with breathing
🔹 Instructions review
- Read the user guide or follow clinician instructions
- Understand how to record and interpret readings
🔹 Consistency
- Perform the test at the same time each day
- Use the same device to track changes accurately
How it’s done
The peak flow test is quick and simple, suitable for home or clinic use:
➡ Step-by-step procedure:
- Reset the meter → Move the indicator to zero
- Stand upright → Take a deep breath in
- Blow out forcefully and quickly → Into the mouthpiece of the peak flow meter
- Record the number → Note the highest reading
- Repeat three times → Record the best of three readings
➡ Tracking results:
- Maintain a peak flow diary
- Compare results to predicted personal best values
- Look for patterns indicating worsening asthma or airway obstruction
💡 Tips for accuracy:
- Use consistent technique each time
- Perform the test before taking bronchodilator medication when possible
- Avoid testing immediately after strenuous exercise
Recovery / Expected Outcomes
Peak flow testing itself is non-invasive and does not require recovery, but the results provide actionable insights:
🔹 Patient benefits:
- Identify early warning signs of asthma flare-ups
- Adjust medications as needed under medical guidance
- Reduce hospital visits or emergency interventions through preventive action
- Enhance patient awareness and confidence in managing respiratory health
🔹 Clinical application:
- Doctors may use peak flow readings to prescribe inhaler adjustments or recommend lifestyle changes
- Regular monitoring helps maintain optimal lung function
Complications / Considerations
The peak flow test is very safe, but some considerations include:
⚠ Incorrect technique → Can lead to misleading readings
⚠ Device malfunction → Dirty or broken meters may produce inaccurate results
⚠ Variability → Factors such as time of day, illness, or fatigue can influence readings
⚠ Over-reliance → Patients should not replace clinical evaluations with home readings alone
Mitigation:
- Ensure proper training for patients
- Use quality-checked devices
- Combine peak flow readings with symptom diaries and medical assessments
Treatment Options in Korea
Peak flow testing is widely available in Korea as part of asthma and respiratory care programs:
🏥 Hospitals and clinics:
- Seoul National University Hospital (SNUH) → Provides asthma management plans including peak flow monitoring
- Asan Medical Center → Offers patient education and home monitoring support
- Samsung Medical Center → Provides integrated respiratory care with peak flow and spirometry testing
- Local community clinics → Often provide peak flow meters and training for asthma patients
💰 Cost and insurance:
- Peak flow meters are affordable and often available for purchase at pharmacies
- Clinical testing may be partially covered by National Health Insurance for asthma management programs
- Private insurance may reimburse home monitoring devices or clinic visits
🔹 Additional support:
- Asthma education programs teach proper technique, recording, and interpretation
- Online apps and diaries help track daily peak flow readings
- Respiratory therapists provide ongoing guidance
Conclusion
The peak flow test in Korea is a simple, reliable, and essential tool for monitoring lung function, especially for patients with asthma or chronic respiratory conditions. By providing early warning signs of airway obstruction, it allows patients and doctors to take preventive measures, adjust treatments, and improve overall respiratory health.