What it is
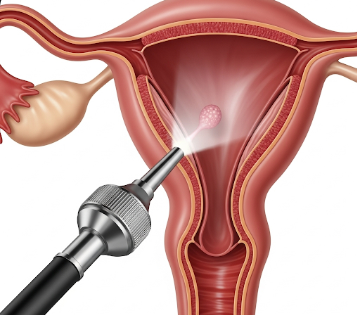
Hysteroscopy is a minimally invasive medical procedure used to examine the inside of the uterus (womb) using a thin, lighted instrument called a hysteroscope. It allows doctors to diagnose and sometimes treat uterine conditions without the need for open surgery.
Key points:
- Used for both diagnostic and operative purposes.
- Can help identify abnormalities such as polyps, fibroids, adhesions, or abnormal bleeding.
- The hysteroscope is usually inserted through the vagina and cervix, eliminating external incisions.
- Can be performed in an outpatient clinic or hospital setting, depending on the procedure’s complexity.
Why it’s done
Hysteroscopy is recommended for a variety of reasons:
- Abnormal uterine bleeding: Heavy, irregular, or postmenopausal bleeding.
- Infertility evaluation: Assessing the uterine cavity before assisted reproductive treatments.
- Uterine fibroids or polyps: Removal or biopsy to prevent further complications.
- Repeated miscarriages: Checking for structural abnormalities like adhesions or septum.
- Intrauterine device (IUD) issues: Locating a displaced or embedded IUD.
- Endometrial biopsy: Obtaining tissue for further testing.
Note: Hysteroscopy allows for both diagnosis and treatment in a single procedure, reducing the need for multiple surgeries.
Alternatives
Other diagnostic or treatment options may include:
- Transvaginal ultrasound: Non-invasive imaging to assess uterine structure.
- Sonohysterography: Ultrasound with fluid to improve visualization of the uterine cavity.
- MRI or CT scans: For complex uterine abnormalities.
- Blind endometrial biopsy: Tissue sampling without direct visualization.
- Open or laparoscopic surgery: In cases where hysteroscopy is insufficient.
Important: Hysteroscopy is usually preferred due to direct visualization, precision, and minimally invasive nature.
Preparation
Proper preparation ensures safety, comfort, and accurate results:
- Consultation: Review medical history, current medications, allergies, and previous surgeries.
- Menstrual cycle timing: Often performed just after menstruation when the uterine lining is thin.
- Medications: Stop blood thinners if advised. Pain relief or mild sedatives may be prescribed.
- Fasting: Usually not required for outpatient hysteroscopy; may be needed for operative procedures under general anesthesia.
- Informed consent: Discuss procedure, risks, benefits, and alternatives.
Patient instructions:
- Empty your bladder before the procedure.
- Arrange for someone to accompany you if sedation is used.
- Wear comfortable clothing and bring sanitary pads for potential spotting.
How it’s done
Hysteroscopy involves several steps depending on whether it is diagnostic or operative:
1. Diagnostic hysteroscopy:
- The patient lies on the examination table with legs in stirrups.
- The hysteroscope is inserted through the vagina and cervix.
- A saline or CO2 solution may be used to expand the uterus for better visibility.
- The doctor examines the uterine lining, openings of the fallopian tubes, and cavity structure.
2. Operative hysteroscopy:
- Similar setup as diagnostic procedure.
- Surgical instruments may be inserted through the hysteroscope to:
- Remove polyps, fibroids, or adhesions.
- Correct structural anomalies such as septum or scar tissue.
- Take biopsy samples for histopathology.
Anesthesia:
- Local, regional, or general anesthesia may be used depending on procedure complexity and patient preference.
Duration:
- Diagnostic hysteroscopy: 5–20 minutes.
- Operative hysteroscopy: 20–60 minutes, depending on intervention.
Recovery
Recovery from hysteroscopy is usually quick and uncomplicated:
- Outpatient procedure: Most patients return home the same day.
- Mild discomfort: Cramping, spotting, or bloating may occur for 1–2 days.
- Activity: Normal activities can usually be resumed within 24–48 hours. Avoid sexual intercourse, tampon use, or heavy lifting for several days if advised.
- Follow-up: Doctor may schedule a visit to review results, check healing, or discuss further treatment.
Benefits of recovery:
- Relief from abnormal bleeding or uterine issues.
- Accurate diagnosis of underlying problems.
- Minimally invasive approach reduces pain, scarring, and recovery time.
Complications
Hysteroscopy is generally safe, but potential risks include:
- Bleeding or spotting: Usually mild and self-limiting.
- Infection: Rare; antibiotics may be prescribed if needed.
- Uterine perforation: Very rare; may require additional intervention.
- Fluid overload: Excess saline absorption in longer procedures.
- Anesthesia-related risks: Only for procedures requiring sedation or general anesthesia.
Prevention:
- Ensure procedure is performed by a qualified gynecologist.
- Follow all pre- and postoperative instructions.
- Report persistent pain, heavy bleeding, or fever immediately.
Treatment Options in Korea
Hysteroscopy is widely available in Korea and offered in public and private hospitals:
Key features:
- Performed in gynecology departments, specialized women’s health centers, and fertility clinics.
- Both diagnostic and operative hysteroscopy are available.
- Korean hospitals use state-of-the-art equipment for high-resolution visualization and minimally invasive intervention.
- Experienced gynecologists provide preoperative counseling, procedure, and follow-up care.
- Post-procedure, patients have access to rehabilitation, counseling, and fertility guidance if needed.
Summary: Hysteroscopy in Korea is a safe, minimally invasive, and highly effective procedure for diagnosing and treating uterine abnormalities. It allows direct visualization, accurate diagnosis, and therapeutic intervention in a single session, with rapid recovery and minimal complications.