What it is
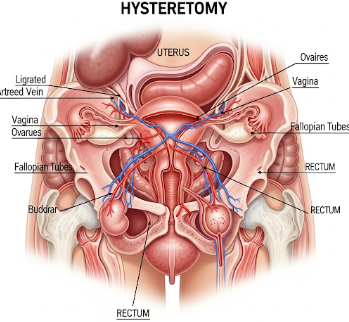
A hysterectomy is a surgical procedure in which a woman’s uterus is removed. Depending on the medical indication, the procedure may also involve the removal of the cervix, fallopian tubes, and ovaries. Hysterectomy is a common treatment for a variety of gynecological conditions and can be life-saving or improve quality of life.
Key points:
- Types include:
- Total hysterectomy: Removal of the uterus and cervix.
- Subtotal (partial/supracervical) hysterectomy: Only the uterus is removed, leaving the cervix.
- Radical hysterectomy: Removal of uterus, cervix, part of the vagina, and surrounding tissues, often for cancer treatment.
- Can be performed using open surgery (abdominal), minimally invasive laparoscopic, or vaginal approaches.
- May be planned (elective) or performed emergently for life-threatening conditions.
Why it’s done
Hysterectomy is recommended for various medical reasons:
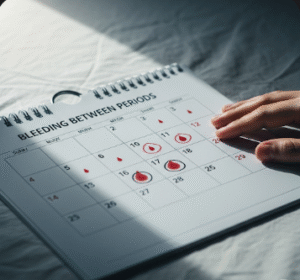
- Uterine fibroids: Large or symptomatic fibroids causing pain, bleeding, or fertility issues.
- Endometriosis: Severe cases where tissue removal relieves chronic pain.
- Uterine prolapse: When the uterus descends into the vaginal canal, causing discomfort.
- Cancer: Treatment for uterine, cervical, or ovarian cancer.
- Abnormal bleeding: When other treatments fail to control heavy menstrual bleeding.
- Chronic pelvic pain: Persistent pain unresponsive to medications or other procedures.
Note: The decision for hysterectomy is carefully evaluated, as it permanently ends fertility and may have hormonal implications.
Alternatives
Before proceeding with hysterectomy, alternatives may include:
- Medications: Hormonal therapy, anti-inflammatory drugs, or medications to control bleeding.
- Minimally invasive procedures: Endometrial ablation, uterine artery embolization, or laparoscopic fibroid removal.
- Lifestyle and supportive measures: Pain management, diet, and physical therapy for symptom relief.
- Fertility-sparing surgeries: Myomectomy or localized excisions for women desiring future pregnancies.
Important: The suitability of alternatives depends on condition severity, patient age, and fertility goals.
Preparation
Proper preparation ensures safety and smooth recovery:
- Preoperative evaluation: Blood tests, imaging (ultrasound, MRI), and anesthesia assessment.
- Medication review: Some medications, like blood thinners, may need to be stopped.
- Fasting instructions: Typically required before surgery.
- Informed consent: Understanding the procedure, risks, recovery, and long-term effects.
- Lifestyle adjustments: Stop smoking, maintain healthy weight, and prepare for postoperative care.
Patient instructions:
- Arrange for postoperative assistance at home.
- Plan for time off work and limitations on physical activity.
- Discuss pain management and hormone replacement therapy if ovaries are removed.
How it’s done
Hysterectomy can be performed using several approaches:
1. Abdominal hysterectomy:
- Incision made in the lower abdomen.
- Allows removal of uterus and surrounding tissues.
- Typically used for large fibroids, cancers, or complex cases.
2. Vaginal hysterectomy:
- Uterus removed through the vagina.
- Minimally invasive with shorter recovery time.
3. Laparoscopic or robotic-assisted hysterectomy:
- Small abdominal incisions with camera and instruments.
- Minimally invasive, shorter hospital stay, and quicker recovery.
4. Radical hysterectomy:
- Used for cancer treatment.
- Removal of uterus, cervix, part of the vagina, and surrounding lymph nodes.
Anesthesia: General or regional anesthesia is used depending on the approach and patient factors.
Recovery
Recovery depends on surgical method and individual health:
- Hospital stay: 1–5 days depending on procedure.
- Initial recovery: 2–6 weeks for minimally invasive surgery, longer for open surgery.
- Activity: Avoid heavy lifting, sexual intercourse, or strenuous exercise until cleared by a doctor.
- Follow-up care: Regular check-ups to monitor healing, manage pain, and detect complications.
- Emotional support: Counseling may help with hormonal changes, loss of fertility, or body image concerns.
Benefits of recovery:
- Relief from pain, bleeding, or prolapse.
- Improved quality of life and daily functioning.
- Resolution of cancer or precancerous conditions if applicable.
Complications
Hysterectomy is generally safe, but risks include:
- Surgical complications: Infection, bleeding, blood clots, or injury to bladder/ureters.
- Anesthesia risks: Rare, but may include adverse reactions.
- Hormonal changes: If ovaries are removed, may cause early menopause.
- Pelvic floor issues: Potential for urinary incontinence or prolapse.
- Emotional impact: Anxiety, depression, or grief due to loss of fertility.
Prevention:
- Choose a qualified surgeon and accredited hospital.
- Follow pre- and postoperative instructions carefully.
- Monitor for signs of infection or complications and seek medical attention promptly.
Treatment Options in Korea
Hysterectomy is widely available in Korea in both public and private healthcare settings:
Key features:
- Performed in general hospitals, women’s health centers, and specialized gynecologic clinics.
- Multiple surgical approaches are offered, including minimally invasive and robotic-assisted techniques.
- Experienced gynecologic surgeons provide preoperative counseling, risk assessment, and postoperative care.
- Post-surgery, Korean hospitals offer rehabilitation, hormonal management, and follow-up care.
- Standardized protocols ensure safety, reduced complications, and quicker recovery.
Summary: Hysterectomy in Korea is a safe and effective treatment for various gynecologic conditions, including fibroids, cancer, and prolapse. When performed by skilled surgeons, it relieves symptoms, improves quality of life, and addresses life-threatening conditions, with structured preoperative preparation and postoperative support ensuring optimal outcomes.