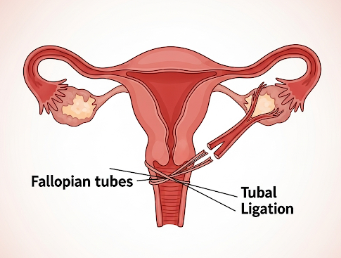
What is Female Sterilisation?
Female sterilisation is a permanent method of contraception that prevents pregnancy by blocking or sealing the fallopian tubes, thus preventing the egg from meeting sperm. It is considered highly effective and long-term, often referred to as tubal ligation.
💡 Key Methods of Female Sterilisation:
✔️ Laparoscopic Tubal Ligation – Small incisions in the abdomen allow the surgeon to access and block the fallopian tubes using clips, rings, or cauterization.
✔️ Hysteroscopic Sterilisation (e.g., Essure) – Non-surgical method where devices are placed into the fallopian tubes via the uterus, causing scarring and blockage (less common now).
✔️ Mini-laparotomy – Small incision surgery, often performed postpartum or after cesarean section.
Purpose:
➡️ Provide a permanent contraception solution
➡️ Reduce risk of unintended pregnancy
➡️ Offer a reliable method for women who have completed their families
In Korea, female sterilisation is performed in hospitals and specialized gynecology clinics, using modern minimally invasive techniques to ensure safety and faster recovery.
Why It’s Done
Female sterilisation is chosen for permanent birth control when other contraceptive methods are unsuitable or undesired.
✔️ Permanent contraception – No need for pills, IUDs, or condoms
✔️ Reliable and effective – Failure rate is extremely low (<1%)
✔️ No hormonal side effects – Unlike oral contraceptives or hormonal IUDs
✔️ Family planning completion – Suitable for women who do not want future pregnancies
✔️ Convenience – Eliminates daily, weekly, or monthly contraceptive management
Clinical Benefits:
➡️ Highly effective – Over 99% effective in preventing pregnancy
➡️ Long-term cost savings – Reduces expense of temporary contraceptives
➡️ Freedom from hormonal effects – No impact on natural menstrual cycles
➡️ Peace of mind – Permanent solution for contraception
In Korea, female sterilisation is recommended after counseling and confirmation of informed consent, ensuring that women understand the permanent nature of the procedure.
Alternatives
Before choosing sterilisation, alternatives include:
⭐ Long-acting reversible contraceptives (LARCs) – IUDs or implants
⭐ Oral contraceptive pills – Daily hormonal contraception
⭐ Barrier methods – Condoms, diaphragms, or cervical caps
⭐ Injectable contraceptives – Hormonal injections lasting 1–3 months
⭐ Natural family planning – Fertility awareness methods
👉 Key Point: Female sterilisation is permanent, while alternatives are reversible and may be more appropriate for women uncertain about future pregnancies.
Preparation
Proper preparation is essential for a safe and successful procedure:
🔹 Medical assessment – Comprehensive evaluation of medical history, allergies, previous surgeries, and reproductive health
🔹 Preoperative tests – Blood tests, ultrasound, and sometimes ECG if under general anesthesia
🔹 Counseling and informed consent – Understanding the procedure, risks, and permanent nature
🔹 Fasting instructions – Usually 6–8 hours before surgery if general anesthesia is planned
🔹 Medication review – Adjustments may be needed for blood thinners or chronic medications
⭐ Arrange post-procedure transport – Patients may not be able to drive after sedation or anesthesia
⭐ Comfortable clothing – Loose attire recommended for post-surgical recovery
How It’s Done
Female sterilisation can be performed using minimally invasive or surgical techniques:
- Laparoscopic Tubal Ligation
✔️ Small abdominal incisions made near the navel
✔️ Laparoscope inserted to visualize fallopian tubes
✔️ Tubes blocked using clips, rings, or cauterization
✔️ Incisions closed with sutures or adhesive strips - Hysteroscopic Sterilisation
🔹 Device inserted through the vagina and uterus into fallopian tubes
🔹 Causes tissue growth that blocks tubes over several weeks
🔹 No abdominal incision required - Mini-laparotomy
➡️ Small incision in lower abdomen, often postpartum
➡️ Tubes are tied, cut, or blocked
➡️ Incision closed with sutures
Highlights:
✔️ Procedure duration – Typically 15–60 minutes
✔️ Anesthesia – Local with sedation or general anesthesia
✔️ Outpatient or short hospital stay – Most patients return home same day or next day
Recovery / Follow-up
Recovery after female sterilisation is generally quick and straightforward:
✔️ Immediate post-op care – Monitoring for vital signs and bleeding
✔️ Pain management – Mild cramping or incision soreness can be managed with analgesics
✔️ Activity restrictions – Avoid heavy lifting or strenuous exercise for 1–2 weeks
✔️ Follow-up appointment – Usually within 1–2 weeks to check incision healing
⭐ Most women resume normal activities within a few days
⭐ Minor bloating, bruising, or fatigue is common but resolves quickly
⭐ No impact on menstrual cycles or hormonal balance
Complications / Risks
Female sterilisation is generally safe, but potential complications include:
⚠️ Surgical risks – Infection, bleeding, or injury to surrounding organs
⚠️ Anesthesia-related complications – Allergic reactions or respiratory issues
⚠️ Failed sterilisation – Very rare; pregnancy can occur if tubes re-canalize
⚠️ Postoperative pain or discomfort – Usually mild and temporary
⚠️ Psychological impact – Some women may experience regret, especially if sterilisation performed at a young age
➡️ In Korea, experienced gynecologists, modern surgical techniques, and sterile operating environments reduce risks substantially.
Treatment Options in Korea
Korean hospitals and clinics offer comprehensive female sterilisation services, including:
🏥 Laparoscopic Tubal Ligation – Most common and minimally invasive
🏥 Postpartum Sterilisation – Mini-laparotomy immediately after cesarean or vaginal delivery
🏥 Hysteroscopic Sterilisation – Non-incisional, outpatient procedure (limited availability)
🏥 Pre- and Post-procedure Counseling – Ensures informed decision-making
🏥 Follow-up and Monitoring – Incision care, complications monitoring, and counseling
Why Korea is a Preferred Destination:
✔️ Highly skilled gynecologists – Experienced in modern sterilisation techniques
✔️ Advanced minimally invasive surgery equipment – Laparoscopic and hysteroscopic tools
✔️ Patient-centered care – Counseling, privacy, and comfort prioritized
✔️ Short hospital stay – Most procedures are outpatient
✔️ Affordable and efficient – Cost-effective care compared to long-term contraceptives in the long run
Approximate Costs in Korea:
🔹 Laparoscopic Tubal Ligation → $800 – $1,500
🔹 Mini-laparotomy (Postpartum) → $600 – $1,200
🔹 Hysteroscopic Sterilisation → $1,000 – $2,000
🔹 Consultation and Follow-up → $50 – $100
Conclusion
Female sterilisation is a safe, permanent, and highly effective contraceptive method.
It helps women:
✔️ Avoid unintended pregnancies permanently
✔️ Reduce the need for daily or periodic contraception
✔️ Experience reliable contraception without hormonal side effects
✔️ Gain convenience and peace of mind
In Korea, women benefit from:
✔️ Advanced minimally invasive surgical techniques
✔️ Expert gynecologists and multidisciplinary support
✔️ Comprehensive pre- and post-procedure counseling
✔️ Safe, cost-effective, and efficient care
👉 Key Message: Female sterilisation in Korea provides permanent, safe, and highly effective contraception, with modern surgical approaches ensuring comfort, safety, and minimal recovery time.