Overview
Blood transfusion is a medical procedure in which donor blood or its components are administered to a patient to replace lost blood, improve oxygen-carrying capacity, or treat specific medical conditions. It is a life-saving intervention in trauma, surgery, anemia, and certain diseases.
Blood transfusions can involve:
- ➤ Whole blood – rarely used; contains all components.
- ➤ Red blood cells (RBCs) – to treat anemia or blood loss.
- ➤ Platelets – to help with clotting disorders.
- ➤ Plasma – contains clotting factors and proteins.
- ➤ Cryoprecipitate – for specific clotting factor deficiencies.
Importance of blood transfusion:
- Restores blood volume and oxygen delivery.
- Prevents shock and organ failure after severe blood loss.
- Supports treatment of cancer, anemia, and clotting disorders.
In South Korea, blood transfusions are performed in hospitals, trauma centers, and specialized clinics with strict safety protocols, including blood typing, crossmatching, and screening for infectious diseases.
Why It’s Done
Blood transfusions are performed to replace or supplement blood components in patients.
Common indications include:
- ➤ Acute blood loss: Trauma, surgery, or internal bleeding.
- ➤ Severe anemia: Due to iron deficiency, chronic disease, or bone marrow disorders.
- ➤ Blood disorders: Sickle cell disease, thalassemia, or hemophilia.
- ➤ Cancer treatment: Chemotherapy may cause anemia or low platelets.
- ➤ Liver disease or clotting disorders: Plasma transfusions provide clotting factors.
- ➤ Critical care: ICU patients often require transfusions for stability.
Benefits for patients:
- ✔️ Restores oxygen-carrying capacity and prevents hypoxia.
- ✔️ Stabilizes blood pressure and circulation.
- ✔️ Reduces risk of organ damage or failure due to blood loss.
Alternatives
In some cases, alternatives may reduce the need for transfusions:
- ➤ Iron supplements: Oral or intravenous iron for iron-deficiency anemia.
- ➤ Erythropoiesis-stimulating agents: Medications that stimulate RBC production.
- ➤ Volume expanders: Saline or plasma expanders for temporary blood volume replacement.
- ➤ Autologous blood donation: Patients donate their own blood before elective surgery.
- ➤ Platelet or clotting factor concentrates: For specific deficiencies.
Key point: While alternatives exist, blood transfusion remains the most direct and effective way to replace lost or deficient blood components in urgent or severe cases.
Preparation
Proper preparation is critical to ensure safety and compatibility.
Steps include:
- ✅ Medical evaluation: History, allergies, and current medications.
- ✅ Blood typing and crossmatching: Ensures donor blood is compatible (ABO and Rh).
- ✅ Consent: Patients are informed about procedure, risks, and benefits.
- ✅ Baseline vital signs: Blood pressure, pulse, temperature, and oxygen saturation.
- ✅ IV access: Large-bore intravenous line inserted for transfusion.
- ✅ Pre-medication (if needed): Antihistamines or antipyretics may be given to prevent reactions.
Important: Screening of donor blood is mandatory in South Korea for HIV, hepatitis B & C, syphilis, and other infectious agents.
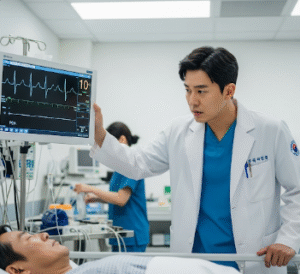
How It’s Done
Blood transfusion is performed under controlled medical supervision.
Step-by-step process:
- Verification: Patient identity, blood type, and crossmatch checked.
- IV insertion: Large-bore needle or catheter inserted into a vein.
- Blood bag preparation: Donor blood checked, warmed if necessary, and connected to IV tubing.
- Transfusion administration:
- Blood is infused slowly initially while monitoring for reactions.
- Rate increased if no adverse reactions occur.
- Monitoring: Continuous observation of vital signs and symptoms.
- Completion: IV line removed, site bandaged, and patient observed for delayed reactions.
Duration: 1–4 hours depending on the type and volume of blood.
Hospital stay: Usually outpatient; longer monitoring for high-risk patients.
Pain level: Minimal; may experience mild discomfort at IV site.
Recovery
Recovery from blood transfusion is typically rapid, with most patients experiencing immediate benefits:
Immediate effects:
- Improved energy and oxygen delivery within hours.
- Stabilization of vital signs and circulation.
- Monitoring for allergic or hemolytic reactions.
Short-term recovery (hours to days):
- Mild fatigue or fever may occur.
- Minor bruising at IV site is common.
- Continued monitoring in hospital or clinic for delayed reactions.
Long-term recovery:
- Blood components replaced within days (platelets) or weeks (RBCs).
- Follow-up tests may be needed to assess hemoglobin, hematocrit, and clotting function.
- Underlying cause of transfusion should be addressed to prevent recurrence.
Possible Complications
While generally safe, blood transfusions carry some risks:
- ⚠️ Allergic reactions: Rash, itching, or fever.
- ⚠️ Fever (febrile non-hemolytic reaction): Mild temperature increase.
- ⚠️ Hemolytic reactions: Rare, serious reaction if blood is incompatible.
- ⚠️ Infections: Very rare due to rigorous donor screening.
- ⚠️ Fluid overload: Especially in heart or kidney disease patients.
- ⚠️ Iron overload: Repeated transfusions may increase iron in the body.
In South Korea, strict protocols, advanced screening, and monitoring have significantly reduced transfusion complications.
Treatment Options / Clinical Relevance in Korea
South Korea provides safe and advanced blood transfusion services across hospitals and blood centers.
Key features:
- 🏥 National blood bank network: Managed by Korea Red Cross, ensuring safe donor blood.
- 🏥 Advanced testing: All blood screened for infectious diseases, ABO and Rh compatibility.
- 🏥 Specialized transfusions: Platelets, plasma, cryoprecipitate, and leukocyte-reduced blood available.
- 🏥 Integration with electronic health records: Ensures traceability and safety.
- 🏥 Emergency services: Rapid transfusion available in trauma centers, ICUs, and surgical units.
Highlights in Korea:
- ✔️ Blood transfusions are highly regulated and safe.
- ✔️ Automated systems minimize human error.
- ✔️ Integration with national health programs ensures availability during emergencies.
- ✔️ Specialized centers provide matched or rare blood types for complex cases.
Highlights
- ➤ Blood transfusion replaces lost or deficient blood components to save lives.
- ➤ Indications include trauma, surgery, anemia, blood disorders, cancer treatment, and organ failure.
- ➤ Preparation includes blood typing, crossmatching, consent, and IV access.
- ➤ Procedure duration is 1–4 hours with continuous monitoring for reactions.
- ➤ Complications are rare, including allergic reactions, hemolysis, infection, or fluid overload.
- ➤ South Korea provides advanced transfusion services, ensuring safety and availability through national blood banks.
- ➤ Timely blood transfusion improves outcomes, stabilizes vital signs, and supports recovery in critical patients.