Overview
Urinary incontinence is the involuntary leakage of urine, affecting people of all ages but more common in women and older adults. It can range from occasional leaks when coughing or sneezing to frequent, uncontrollable urination that significantly impacts daily life.
➤ Urinary incontinence is a symptom, not a disease, often linked to bladder dysfunction, pelvic floor weakness, or neurological disorders.
➤ It can affect physical, emotional, and social well-being, causing embarrassment, anxiety, and reduced quality of life.
➤ In Korea, urology and gynecology centers offer comprehensive evaluation and multidisciplinary treatment to manage urinary incontinence effectively.
Key Facts
► Definition: Loss of bladder control resulting in urine leakage.
► Prevalence: Affects millions worldwide, with higher rates in women and elderly adults.
► Types: Stress, urge, overflow, functional, and mixed incontinence.
► Risk factors: Pregnancy, childbirth, menopause, obesity, neurological disorders, prostate enlargement.
► Treatment in Korea: Medical management, pelvic floor therapy, minimally invasive surgery, and lifestyle interventions.
What is Urinary Incontinence?
Urinary incontinence occurs when the bladder loses the ability to store or release urine properly. It may result from:
➔ Weakness in the pelvic floor muscles supporting the bladder and urethra.
➔ Overactive bladder muscles causing urine leakage with sudden urge.
➔ Neurological conditions affecting nerve signals to the bladder.
➔ Structural issues like enlarged prostate in men or pelvic organ prolapse in women.
This condition can be temporary or chronic, depending on the underlying cause. Early identification and treatment can prevent progression and improve quality of life.
What Symptoms Are Related to Urinary Incontinence?
Urinary incontinence often presents with symptoms that vary depending on the type:
→ Stress incontinence: Leakage during coughing, sneezing, laughing, or exercise.
→ Urge incontinence: Sudden, intense urge to urinate, often leading to leakage.
→ Overflow incontinence: Frequent dribbling due to incomplete bladder emptying.
→ Functional incontinence: Leakage due to physical or cognitive impairments preventing timely bathroom use.
→ Mixed incontinence: Combination of stress and urge symptoms.
Other associated signs may include:
► Frequent urination (more than 8 times per day).
► Nocturia (waking at night to urinate).
► Burning or discomfort during urination (dysuria), if infection is present.
► Pelvic pressure or prolapse in women.
► Weak urine stream in men with prostate issues.
Causes / Possible Causes of Urinary Incontinence
Pelvic Floor Weakness (Women)
➤ Pregnancy, childbirth, and menopause can weaken pelvic muscles.
➤ Pelvic organ prolapse increases bladder pressure and contributes to leakage.
Bladder-Related Causes
➔ Overactive bladder (OAB) – involuntary bladder contractions causing urgency.
➔ Chronic urinary tract infections (UTIs) – irritate bladder lining, increasing leakage.
Neurological Causes
→ Stroke, Parkinson’s disease, multiple sclerosis, or spinal cord injuries can disrupt bladder nerve control.
→ Nerve damage from diabetes may also contribute.
Prostate-Related Causes (Men)
► Benign prostatic hyperplasia (BPH) causing bladder outlet obstruction.
► Prostate surgery can sometimes lead to temporary or persistent incontinence.
Other Contributing Factors
➤ Medications, including diuretics or sedatives.
➤ Obesity increasing abdominal pressure on the bladder.
➤ Chronic coughing or respiratory conditions exerting repeated pressure on the bladder.
When Should I See My Doctor?
Medical evaluation is recommended if urinary incontinence:
➤ Interferes with daily activities, sleep, or social life.
➤ Occurs suddenly or worsens rapidly.
➤ Is accompanied by pain, burning, blood in urine, or fever.
➤ Causes skin irritation, infection, or sores due to leakage.
➤ Persists despite lifestyle changes or pelvic floor exercises.
Early consultation allows targeted treatment, preventing complications, and improving quality of life.
Care and Treatment
Lifestyle and Behavioral Measures
► Maintain a healthy weight to reduce bladder pressure.
► Limit caffeine, alcohol, and bladder irritants.
► Establish a timed voiding schedule to prevent leakage.
► Practice pelvic floor exercises (Kegels) to strengthen support muscles.
► Avoid constipation, which increases abdominal pressure on the bladder.
Medical Treatments
➔ Medications: Antimuscarinics or beta-3 agonists for overactive bladder.
➔ Topical estrogen therapy for postmenopausal women with urethral atrophy.
➔ Antibiotics for recurrent UTIs.
➔ Alpha-blockers or 5-alpha-reductase inhibitors for men with prostate enlargement.
Advanced and Surgical Interventions
→ Minimally invasive sling procedures for stress incontinence.
→ Bladder Botox injections for severe overactive bladder.
→ Neuromodulation therapy (sacral nerve stimulation) for refractory incontinence.
→ Prostate surgery or corrective pelvic surgery when structural issues are present.
Treatment Options in Korea
South Korea provides comprehensive, multidisciplinary care for urinary incontinence, combining urology, gynecology, physiotherapy, and advanced surgery.
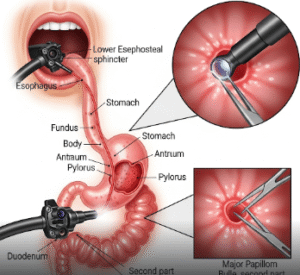
Diagnosis in Korea
➤ Urinalysis, urine culture, and blood tests to rule out infection or metabolic causes.
➤ Imaging: Ultrasound, CT, or MRI for structural assessment.
➤ Urodynamic studies to evaluate bladder and sphincter function.
Non-Surgical Care
► Pelvic floor therapy with guided exercises.
► Behavioral interventions including bladder training.
► Medications tailored to overactive bladder or prostate issues.
Surgical & Advanced Interventions
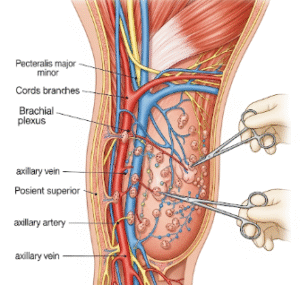
➔ Sling or tape procedures for women with stress incontinence.
➔ Robotic-assisted surgery for prostate-related incontinence.
➔ Neuromodulation and Botox for severe, refractory cases.
Rehabilitation and Lifestyle Support
→ Ongoing follow-up and symptom monitoring.
→ Education on bladder health and lifestyle modifications.
→ Support programs to improve quality of life and emotional well-being.
Korean hospitals integrate advanced technology, expert specialists, and patient-centered care, ensuring effective management of urinary incontinence.