➤ Overview
Tachypnea is a medical term used to describe abnormally rapid breathing. It is a common symptom in both children and adults and can indicate underlying respiratory, cardiac, metabolic, or systemic conditions. Rapid breathing is often the body’s attempt to increase oxygen intake or remove excess carbon dioxide.
In South Korea, tachypnea is assessed by pulmonologists, cardiologists, and emergency medicine specialists. Early evaluation is crucial for diagnosing the underlying cause, preventing complications, and initiating appropriate treatment.
➤ Key Facts
→ Tachypnea refers to respiratory rates above the normal range – typically >20 breaths per minute in adults and higher in children depending on age.
→ It may occur suddenly or gradually, depending on the cause.
→ Tachypnea can be painful, uncomfortable, or asymptomatic, but persistent rapid breathing always warrants evaluation.
→ Common triggers include respiratory infections, asthma, heart failure, metabolic disorders, and anxiety.
→ In Korea, diagnosis often involves physical examination, vital sign monitoring, imaging, and laboratory tests.
→ Early recognition prevents hypoxia, respiratory failure, and other life-threatening complications.
→ Treatment targets both the underlying cause and symptomatic relief.
➤ What is Tachypnea?
Tachypnea is defined as rapid, shallow, or sometimes deep breathing exceeding the normal rate for a person’s age:
→ Physiological tachypnea – Temporary increase due to exercise, stress, or high altitude.
→ Pathological tachypnea – Resulting from medical conditions such as pneumonia, heart failure, or sepsis.
→ Shallow tachypnea – Rapid breathing with small breaths, often seen in restrictive lung disease.
→ Kussmaul respiration – Deep, rapid breathing associated with metabolic acidosis (e.g., diabetic ketoacidosis).
→ Cheyne-Stokes respiration – Cycles of rapid and slow breathing, often seen in heart failure or neurological conditions.
In South Korea, clinicians differentiate tachypnea types using age-based respiratory rates, oxygen saturation, and associated clinical signs.
➤ What Symptoms are Related to Tachypnea?
Tachypnea is often accompanied by other respiratory, cardiovascular, or systemic symptoms:
→ Shortness of breath → Difficulty catching breath during rest or activity.
→ Chest discomfort or pain → May indicate cardiac or pulmonary involvement.
→ Cough or sputum production → Often present in respiratory infections.
→ Wheezing or noisy breathing → Associated with asthma or airway obstruction.
→ Fatigue or weakness → Due to increased energy demand and oxygen use.
→ Cyanosis → Bluish discoloration of lips or extremities, indicating hypoxia.
→ Dizziness or lightheadedness → Caused by reduced oxygen delivery to the brain.
→ Fever → May accompany infections causing tachypnea.
→ Rapid heartbeat (tachycardia) → Common with anxiety, fever, or cardiac issues.
→ Sweating and anxiety → Often present in acute respiratory distress.
➤ What Causes / Possible Causes?
Tachypnea may result from respiratory, cardiac, metabolic, neurological, or psychological conditions:
→ Respiratory causes – Pneumonia, asthma, chronic obstructive pulmonary disease (COPD), pulmonary embolism.
→ Cardiac causes – Heart failure, myocardial infarction, or congenital heart defects in children.
→ Metabolic causes – Diabetic ketoacidosis, sepsis, or acidosis.
→ Fever or infection – Increases metabolic demand and breathing rate.
→ Pain or trauma – Post-surgical, rib fractures, or abdominal pain causing rapid breathing.
→ Anemia – Reduced oxygen-carrying capacity leads to compensatory tachypnea.
→ Anxiety or panic attacks – Hyperventilation can cause rapid breathing.
→ Neurological causes – Brain injury, stroke, or raised intracranial pressure.
→ Medications or toxins – Stimulants, salicylate poisoning, or other drugs affecting respiratory drive.
➤ When Should I See My Doctor?
Immediate medical attention is required if tachypnea is persistent, severe, or accompanied by warning signs:
→ Rapid breathing at rest or with minimal exertion.
→ Shortness of breath, chest pain, or palpitations.
→ Bluish lips or fingertips indicating low oxygen levels.
→ Fever or signs of infection with rapid breathing.
→ Sudden onset following trauma or suspected pulmonary embolism.
→ Confusion, dizziness, or fainting accompanying tachypnea.
→ Difficulty speaking or severe respiratory distress.
→ Underlying chronic conditions such as heart or lung disease worsening.
Early evaluation in Korea ensures timely diagnosis, emergency care if needed, and targeted treatment.
➤ Care and Treatment
Treatment focuses on addressing the underlying cause while providing symptomatic relief:
→ Oxygen therapy – For hypoxia or respiratory distress.
→ Medications – Bronchodilators, antibiotics, diuretics, or antipyretics depending on cause.
→ Fluid management – For dehydration, sepsis, or metabolic disturbances.
→ Positioning and breathing techniques – Sitting upright or pursed-lip breathing to ease airflow.
→ Pain management – Analgesics if tachypnea is related to trauma or surgery.
→ Lifestyle adjustments – Smoking cessation, weight management, and exercise for chronic conditions.
→ Monitoring – Continuous assessment of oxygen saturation, respiratory rate, and vital signs.
→ Hospitalization – In severe or life-threatening cases requiring intensive care.
➤ Treatment Options in Korea
South Korea provides advanced diagnostics and treatment options for tachypnea:
Diagnosis in Korea
→ Physical examination – Assessment of breathing pattern, rate, and effort.
→ Vital signs monitoring – Oxygen saturation, heart rate, and blood pressure.
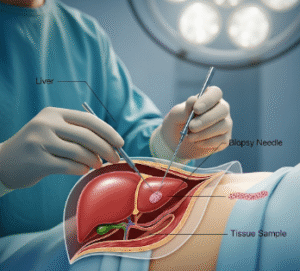
→ Imaging – Chest X-ray, CT scan, or ultrasound for respiratory and cardiac evaluation.
→ Laboratory tests – Blood gas analysis, complete blood count, and metabolic panels.
→ Electrocardiography (ECG) – To assess cardiac involvement.
Medical Treatments in Korea
→ Pharmacological therapy – Antibiotics, bronchodilators, steroids, or diuretics based on diagnosis.
→ Oxygen supplementation – Via nasal cannula, mask, or high-flow devices.
→ Supportive care – Intravenous fluids, fever management, and nutrition support.
Advanced Therapies in Korea
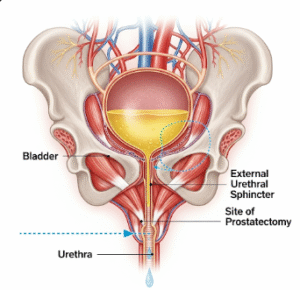
→ Mechanical ventilation – Non-invasive or invasive support for severe respiratory failure.
→ Pulmonary rehabilitation programs – For chronic respiratory diseases.
→ Critical care interventions – ICU support for severe infections, sepsis, or cardiac failure.
→ Minimally invasive procedures – For pulmonary embolism or cardiac causes if indicated.
Rehabilitation & Support in Korea
→ Education on breathing exercises, medication adherence, and lifestyle modifications.
→ Follow-up to monitor lung and heart function, prevent recurrence, and manage chronic conditions.
→ Integration with pulmonology, cardiology, and rehabilitation specialists for holistic care.