➤ Overview
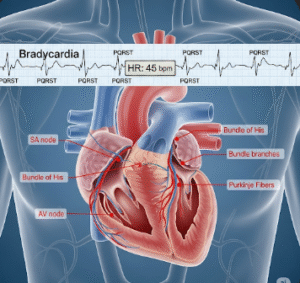
Tachycardia refers to an abnormally fast heart rate, usually defined as more than 100 beats per minute in adults. It can occur as a normal physiological response to exercise, stress, or excitement, but it may also indicate underlying heart conditions or systemic illness.
In South Korea, tachycardia evaluation is conducted by cardiologists and primary care physicians. Diagnostic testing, including ECG (electrocardiogram), Holter monitoring, echocardiography, and blood tests, helps determine the cause and severity. Early diagnosis is essential to manage symptoms, prevent complications, and reduce the risk of cardiovascular events.
➤ Key Facts
→ Tachycardia can be physiological (normal) or pathological (abnormal).
→ Common triggers include stress, fever, exercise, caffeine, or stimulant medications.
→ Pathological causes include arrhythmias, heart disease, thyroid disorders, anemia, or electrolyte imbalances.
→ In Korea, advanced cardiac diagnostics like Holter monitoring and echocardiography are standard.
→ Symptoms may vary from palpitations, dizziness, shortness of breath, to chest pain.
→ Early intervention prevents heart failure, stroke, or sudden cardiac events.
→ Management may involve lifestyle modification, medications, or invasive cardiac procedures.
➤ What is Tachycardia?
Tachycardia is a condition characterized by an elevated heart rate:
→ Resting heart rate >100 bpm in adults is typically considered tachycardia.
→ Physiological tachycardia – Normal response to exercise, stress, or excitement.
→ Pathological tachycardia – Caused by arrhythmias or underlying medical conditions.
→ Types of tachycardia –
→ Supraventricular tachycardia (SVT) – Rapid heartbeat originating above the ventricles.
→ Ventricular tachycardia (VT) – Rapid heartbeat originating in the ventricles, potentially life-threatening.
→ Sinus tachycardia – Normal response to stimuli like fever, anxiety, or anemia.
→ Impact on health – Persistent tachycardia can lead to heart failure, blood clots, or fainting episodes.
➤ What Symptoms are Related to Tachycardia?
Symptoms depend on the type and severity of tachycardia:
→ Palpitations → Feeling of racing, pounding, or fluttering heartbeat.
→ Dizziness or lightheadedness → Due to reduced blood flow to the brain.
→ Shortness of breath → Especially during exertion or when lying down.
→ Chest pain or discomfort → May indicate underlying heart disease.
→ Fatigue or weakness → Result of inefficient heart pumping.
→ Fainting or near-fainting episodes → Syncope from insufficient blood supply.
→ Rapid pulse felt in the neck or chest → Especially during episodes of SVT.
→ Sweating or anxiety → Common physiological response to rapid heart rate.
➤ What Causes / Possible Causes?
Tachycardia can result from heart-related, systemic, or external factors:
→ Cardiac causes – Arrhythmias, heart failure, cardiomyopathy, congenital heart defects.
→ Metabolic or systemic causes – Hyperthyroidism, anemia, dehydration, fever, electrolyte imbalances.
→ Medications or stimulants – Caffeine, nicotine, decongestants, or illicit drugs.
→ Stress or anxiety – Sympathetic nervous system activation.
→ Infections – Sepsis or systemic infection causing increased heart rate.
→ Pulmonary conditions – Pulmonary embolism, chronic lung disease, hypoxia.
→ Post-surgical or post-traumatic states – Increased heart rate as a compensatory mechanism.
→ Autonomic dysfunction – Disorders affecting heart rate regulation, such as POTS.
➤ When Should I See My Doctor?
Medical evaluation is essential if tachycardia is:
→ Persistent or recurrent at rest – Not explained by exercise, stress, or caffeine.
→ Accompanied by chest pain, shortness of breath, or fainting – Potentially life-threatening.
→ Associated with palpitations that worsen or disrupt daily activities – Needs specialist assessment.
→ Linked to underlying conditions – Such as hyperthyroidism, anemia, or heart disease.
→ Rapid ventricular tachycardia or irregular pulse – Requires urgent cardiology evaluation.
→ In Korea, cardiologists use ECG, Holter monitoring, echocardiography, and blood tests for accurate diagnosis and treatment planning.
➤ Care and Treatment
Treatment depends on cause, severity, and type of tachycardia:
→ Lifestyle modifications → Reduce caffeine, alcohol, nicotine, manage stress, maintain hydration.
→ Medications → Beta-blockers, calcium channel blockers, or antiarrhythmic drugs.
→ Treat underlying conditions – Correct anemia, hyperthyroidism, electrolyte imbalance, or infection.
→ Vagal maneuvers – Techniques like the Valsalva maneuver for SVT.
→ Catheter ablation – For recurrent or severe arrhythmias not responsive to medications.
→ Cardioversion – Electrical shock therapy for certain types of dangerous tachycardia.
→ Monitoring and follow-up – Regular ECGs, Holter monitoring, and check-ups to prevent complications.
➤ Treatment Options in Korea
South Korea provides advanced cardiac care and interventions for tachycardia:
Diagnosis in Korea
→ Electrocardiogram (ECG) – Detects arrhythmias and heart rate abnormalities.
→ Holter monitoring – Continuous ECG monitoring over 24–72 hours.
→ Echocardiography – Evaluates heart structure and function.
→ Blood tests – Check thyroid function, electrolytes, and systemic conditions.
→ Stress tests – Assess heart response to exertion.
Medical Treatments in Korea
→ Medications – Beta-blockers, calcium channel blockers, antiarrhythmic drugs, or anticoagulants if needed.
→ Lifestyle interventions – Diet modification, stress management, and exercise recommendations.
→ Non-invasive therapies – Vagal maneuvers or biofeedback techniques for mild cases.
Advanced Therapies in Korea
→ Catheter ablation – Minimally invasive procedure to correct arrhythmias.
→ Cardioversion – Electrical therapy for acute tachycardia episodes.
→ Implantable devices – Pacemakers or ICDs for severe or recurrent arrhythmias.
→ Multidisciplinary cardiac care – Cardiologists, electrophysiologists, and nutritionists collaborate for optimal outcomes.
Rehabilitation & Support in Korea
→ Regular cardiac monitoring to prevent recurrence.
→ Lifestyle and dietary guidance for heart health and long-term prevention.
→ Patient education programs on recognizing symptoms, avoiding triggers, and adhering to treatment.