➤ Overview
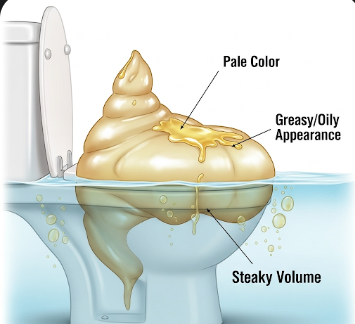
Steatorrhea is a medical condition characterized by excess fat in the stool, which often makes stools bulky, pale, foul-smelling, and difficult to flush. It usually indicates malabsorption in the digestive system, meaning the body is unable to properly absorb fats from food.
In South Korea, steatorrhea is assessed by gastroenterologists, nutritionists, and primary care physicians. Early evaluation and treatment are important to identify underlying conditions, prevent nutrient deficiencies, and maintain digestive health.
➤ Key Facts
→ Steatorrhea is a sign of fat malabsorption, not a disease itself.
→ Stools often appear pale, greasy, and float due to high fat content.
→ Common causes include pancreatic disorders, liver disease, bile duct obstruction, or intestinal disorders.
→ In Korea, advanced diagnostic tests such as stool fat analysis, imaging, and endoscopy are widely available.
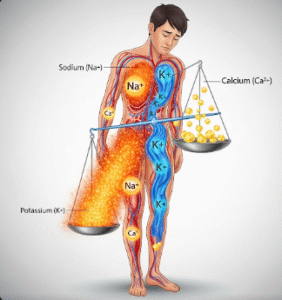
→ Persistent steatorrhea can lead to vitamin deficiencies (A, D, E, K) and weight loss.
→ Treatment focuses on managing the underlying cause and improving nutrient absorption.
→ Dietary modifications and medications may help reduce fat content in stools and improve digestive function.
➤ What is Steatorrhea?
Steatorrhea is defined as excessive fat excretion in the stool, resulting from inadequate digestion or absorption of dietary fats.
→ Malabsorption-related steatorrhea – Occurs when the small intestine cannot absorb fats due to conditions like celiac disease or Crohn’s disease.
→ Pancreatic insufficiency-related steatorrhea – Caused by inadequate pancreatic enzymes needed for fat digestion.
→ Liver or bile-related steatorrhea – Insufficient bile production or obstruction of bile ducts affects fat emulsification.
→ Chronic or acute – Can range from temporary fat malabsorption to chronic gastrointestinal disease.
Korean gastroenterologists carefully assess medical history, stool characteristics, and digestive function to determine the cause and guide treatment.
➤ What Symptoms are Related to Steatorrhea?
Steatorrhea often occurs alongside other digestive and systemic symptoms, which help identify its underlying cause:
→ Bulky, pale, greasy stools that may float.
→ Foul or rancid-smelling stools due to unabsorbed fat.
→ Abdominal discomfort, bloating, or cramping.
→ Diarrhea or frequent loose stools.
→ Weight loss despite normal or increased food intake.
→ Fatigue or weakness due to nutrient malabsorption.
→ Vitamin deficiencies – Night blindness, easy bruising, or bone pain from fat-soluble vitamin deficiency.
→ Nausea or loss of appetite in some cases.
➤ What Causes / Possible Causes?
Steatorrhea arises from conditions affecting fat digestion or absorption:
→ Chronic pancreatitis – Reduced enzyme production leading to fat malabsorption.
→ Cystic fibrosis – Genetic disorder causing pancreatic insufficiency.
→ Celiac disease – Autoimmune reaction to gluten damaging the small intestine.
→ Crohn’s disease – Inflammatory bowel disease affecting nutrient absorption.
→ Bile acid deficiency or bile duct obstruction – Liver disease or gallstones impair fat emulsification.
→ Short bowel syndrome – After surgical removal of parts of the small intestine.
→ Medications – Orlistat or other fat-blocking drugs.
→ Infections – Chronic parasitic or bacterial infections affecting digestion.
➤ When Should I See My Doctor?
Medical evaluation is necessary if steatorrhea is persistent, severe, or associated with other concerning symptoms:
→ Stools consistently pale, greasy, or foul-smelling over several weeks.
→ Unexplained weight loss or malnutrition.
→ Signs of vitamin deficiencies – Night blindness, bone pain, or easy bruising.
→ Persistent abdominal pain, bloating, or diarrhea.
→ Blood in stool or other alarming gastrointestinal signs.
→ History of chronic liver, pancreatic, or intestinal disease.
→ Symptoms not responding to dietary adjustments or medications.
➤ Care and Treatment
Treatment of steatorrhea focuses on addressing the underlying cause, improving fat digestion, and preventing nutrient deficiencies:
→ Dietary modifications – Low-fat diet, medium-chain triglycerides (MCTs), and balanced nutrition.
→ Pancreatic enzyme replacement therapy – For pancreatic insufficiency.
→ Bile acid supplementation – For bile-related malabsorption.
→ Treatment of underlying gastrointestinal disease – Celiac disease, Crohn’s disease, or infections.
→ Vitamin supplementation – Fat-soluble vitamins A, D, E, K.
→ Hydration and electrolyte support – For patients with chronic diarrhea.
→ Avoiding medications that worsen fat absorption unless prescribed.
→ Regular follow-up and stool monitoring to track improvement.
➤ Treatment Options in Korea
South Korea offers advanced evaluation and management for steatorrhea, integrating gastroenterology, nutrition, and advanced therapies:
Diagnosis in Korea
→ Stool fat analysis to quantify fat content.
→ Endoscopy or colonoscopy to evaluate intestinal mucosa and absorption.
→ Imaging studies (ultrasound, CT, MRI) to assess pancreas, liver, and bile ducts.
→ Blood tests to check for nutrient deficiencies and pancreatic function.
Medical Treatments in Korea
→ Prescription pancreatic enzymes or bile acid supplements.
→ Medications to manage underlying inflammatory or autoimmune conditions.
→ Nutritional counseling and personalized dietary plans.
Advanced Therapies in Korea
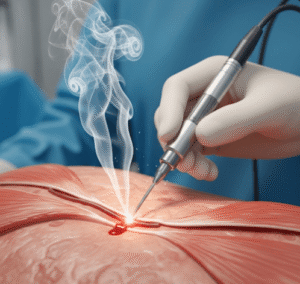
→ Endoscopic or surgical interventions for bile duct obstruction or chronic pancreatitis complications.
→ Integrative approaches combining Western medicine with Korean traditional treatments for digestive health and symptom relief.
→ Ongoing monitoring and rehabilitative nutrition therapy for chronic malabsorption.
Rehabilitation & Support in Korea
→ Education on dietary fat management and symptom tracking.
→ Follow-up to ensure nutrient absorption and recovery.
→ Support for long-term digestive health and prevention of recurrence.