➤ Overview
Shaking, also called tremors, refers to involuntary, rhythmic movements of the body or body parts, most commonly affecting the hands, arms, legs, or head. It can range from mild, barely noticeable trembling to severe, disabling movements.
In South Korea, shaking is assessed by neurologists, movement disorder specialists, and endocrinologists. Early evaluation helps identify the underlying cause, prevent complications, and guide appropriate treatment, improving quality of life and functional independence.
➤ Key Facts
→ Shaking can be temporary or chronic, depending on its cause.
→ Commonly affects hands, arms, head, legs, or voice.
→ In Korea, neurological examinations, blood tests, and imaging are routinely used to determine the cause.
→ Shaking may be associated with stress, fatigue, neurological disorders, or metabolic conditions.
→ Certain medications or substances (e.g., caffeine, alcohol withdrawal) can trigger tremors.
→ Tremors may worsen with age or underlying neurological disease.
→ Early diagnosis improves treatment outcomes, daily function, and safety.
➤ What is Shaking?
Shaking is caused by involuntary muscle contractions or abnormal nerve signaling. It is classified based on pattern, timing, and trigger:
→ Resting tremor – Occurs when muscles are relaxed; often seen in Parkinson’s disease.
→ Action tremor – Appears during voluntary movements such as writing, eating, or holding objects.
→ Postural tremor – Occurs while maintaining a position against gravity, e.g., arms outstretched.
→ Intention tremor – Worsens as the hand approaches a target; often linked to cerebellar disorders.
→ Physiologic tremor – Mild shaking seen in healthy individuals, often exacerbated by stress, fatigue, or caffeine.
Korean neurologists assess severity, frequency, and impact on daily activities to differentiate benign tremors from pathological causes.
➤ What Symptoms are Related to Shaking?
Shaking may present with various associated symptoms depending on the cause:
→ Visible trembling or quivering of hands, arms, legs, head, or voice.
→ Difficulty performing fine motor tasks, such as writing, buttoning clothes, or using utensils.
→ Muscle stiffness or weakness in some neurological conditions.
→ Balance or coordination problems, particularly with cerebellar involvement.
→ Fatigue or worsening tremors with prolonged activity.
→ Associated anxiety, stress, or panic symptoms, exacerbating tremors.
→ Changes in gait or posture if tremor affects lower limbs.
→ Numbness or tingling, when tremor is linked to neuropathy.
➤ What Causes / Possible Causes?
Shaking can result from neurological, metabolic, or external factors:
→ Essential tremor – A common, usually hereditary movement disorder causing action tremors.
→ Parkinson’s disease – Resting tremor with stiffness, slowed movements, and balance issues.
→ Hyperthyroidism – Overactive thyroid accelerates metabolism, causing hand tremors.
→ Medications or stimulants – Caffeine, corticosteroids, or certain asthma medications.
→ Neuropathy – Nerve damage from diabetes, toxins, or autoimmune disorders.
→ Fatigue or anxiety – Stress-induced or physiologic tremors.
→ Alcohol withdrawal – Tremors during detoxification.
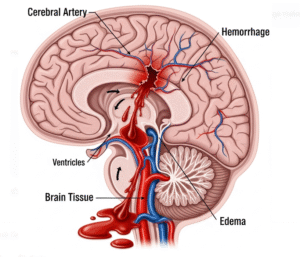
→ Cerebellar disorders or stroke – Intention tremors and coordination deficits.
→ Metabolic imbalances – Low blood sugar, electrolyte disturbances, or liver/kidney dysfunction.
➤ When Should I See My Doctor?
Medical attention is essential if shaking is persistent, worsening, or interfering with daily life:
→ Tremors that interfere with work, eating, or writing.
→ Sudden-onset tremors or tremors accompanied by weakness, numbness, or facial drooping.
→ Resting tremors suggestive of Parkinson’s disease.
→ Tremors associated with dizziness, imbalance, or falls.
→ Shaking with other neurological symptoms, such as speech changes or vision problems.
→ Medication-induced tremors or substance withdrawal.
→ Tremors accompanied by palpitations, sweating, or weight changes, suggesting metabolic or endocrine causes.
➤ Care and Treatment
Treatment depends on cause, severity, and impact on daily life:
→ Medications – Beta-blockers, anticonvulsants, or Parkinson’s drugs for specific tremors.
→ Lifestyle modifications – Reducing caffeine, managing stress, and ensuring adequate rest.
→ Physical or occupational therapy – Improves coordination, strength, and fine motor skills.
→ Assistive devices – Weighted utensils, braces, or ergonomic tools for daily tasks.
→ Surgery or advanced interventions – Deep brain stimulation (DBS) or focused ultrasound for severe, treatment-resistant tremors.
→ Treatment of underlying conditions – Thyroid regulation, diabetes management, or discontinuing causative medications.
→ Supportive care – Counseling or support groups to address anxiety and daily living challenges.
→ Monitoring progression – Regular neurologist follow-ups to track symptom changes and adjust therapy.
➤ Treatment Options in Korea
South Korea offers state-of-the-art neurological and rehabilitative care for tremors:
Diagnosis in Korea
→ Neurological examinations to assess tremor type, amplitude, and frequency.
→ Blood tests for thyroid function, electrolytes, and metabolic causes.
→ Imaging: MRI or CT scans to rule out structural brain abnormalities.
→ Electromyography (EMG) and accelerometry to quantify tremor patterns.
Medical Treatments in Korea
→ Prescription beta-blockers or anticonvulsants for essential tremor.
→ Parkinson’s medications for tremors related to neurodegeneration.
→ Adjusting causative medications under physician guidance.
→ Physical therapy programs for motor skill training.
Advanced Therapies in Korea
→ Deep brain stimulation (DBS) for severe, treatment-resistant tremors.
→ Focused ultrasound therapy – Non-invasive technique to reduce tremor amplitude.
→ Multidisciplinary care – Neurology, rehabilitation, and occupational therapy.
→ Integrative approaches – Korean traditional medicine techniques for supportive symptom management.
Rehabilitation & Support in Korea
→ Guidance on daily activity adaptation, tremor management, and assistive device usage.
→ Counseling for emotional well-being and stress reduction.
→ Long-term follow-up to monitor disease progression and optimize therapy.