➤ Overview
Loss or change in the sense of smell, medically termed anosmia (complete loss) or hyposmia / dysosmia (partial loss or altered perception), can significantly impact taste, nutrition, safety, and quality of life. This condition may occur suddenly or gradually, affecting one or both nostrils.
In South Korea, ENT specialists and neurologists assess changes in smell using nasal endoscopy, smell tests, and imaging studies. Early evaluation is crucial to identify reversible causes, manage underlying conditions, and prevent complications such as malnutrition or exposure to hazards (e.g., gas leaks).
➤ Key Facts
→ Loss of smell can be temporary or permanent, depending on cause.
→ It often impacts taste, leading to reduced appetite or altered dietary habits.
→ In Korea, COVID-19 has been a common cause of temporary anosmia in recent years.
→ Causes range from nasal obstruction, infection, neurological disorders, to trauma.
→ Chronic anosmia can affect mental health, contributing to depression or social isolation.
→ Smell dysfunction can be an early sign of neurodegenerative diseases like Parkinson’s or Alzheimer’s.
→ Prompt evaluation improves the chance of restoring olfactory function.
➤ What is Loss or Change in Sense of Smell?
A reduced or altered sense of smell occurs when olfactory receptors, nerves, or brain regions responsible for olfaction are impaired:
→ Anosmia – Complete inability to detect odors.
→ Hyposmia – Partial loss, reduced sensitivity to smells.
→ Parosmia – Distorted perception of odors (e.g., pleasant smells perceived as foul).
→ Phantosmia – Perception of smells when none are present (olfactory hallucinations).
Korean ENT physicians evaluate both peripheral causes (nasal passages, sinuses) and central causes (brain-related issues) to determine the mechanism.
➤ What Symptoms are Related to Loss or Change in Smell?
Changes in olfaction can present with various associated symptoms:
→ Reduced or absent ability to detect odors in daily life.
→ Altered taste perception, since smell and taste are closely linked.
→ Difficulty enjoying food or detecting spoiled items.
→ Distorted smells (parosmia) or phantom odors (phantosmia).
→ Nasal congestion, runny nose, or sinus pressure if caused by infection.
→ Headaches or facial pressure in sinus-related causes.
→ Loss of appetite or weight changes due to impaired taste.
→ Emotional impact – frustration, anxiety, or depressive symptoms.
➤ What Causes / Possible Causes?
Loss or change in smell may result from local nasal issues, neurological disorders, infections, or systemic factors:
→ Upper respiratory infections – Common cold, influenza, or COVID-19.
→ Sinus disease – Chronic rhinosinusitis, nasal polyps, or allergies.
→ Head trauma – Injury damaging olfactory nerves or brain regions.
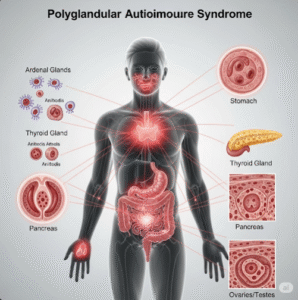
→ Neurological disorders – Parkinson’s disease, Alzheimer’s disease, multiple sclerosis.
→ Exposure to toxins – Smoking, chemical inhalation, or environmental irritants.
→ Aging – Gradual decline in olfactory function with age.
→ Medications – Some antibiotics, antihistamines, or chemotherapy agents.
→ Congenital anosmia – Rare condition present from birth.
➤ When Should I See My Doctor?
Medical consultation is recommended if olfactory changes are persistent, sudden, or affecting quality of life:
→ Sudden loss of smell – May indicate viral infection or neurological issue.
→ Persistent anosmia lasting more than a few weeks.
→ Distorted or phantom smells interfering with daily life.
→ Associated nasal blockage, bleeding, or chronic congestion.
→ Neurological symptoms – Weakness, numbness, memory loss, or tremors.
→ Impact on eating, safety, or mental health.
→ Post-trauma or surgery changes in smell requiring assessment.
➤ Care and Treatment
Treatment depends on the underlying cause and severity of olfactory dysfunction:
→ Addressing nasal obstruction – Removal of polyps, sinus surgery, or allergy management.
→ Treating infections – Antibiotics or antiviral medications for bacterial or viral causes.
→ Olfactory training – Structured smell exercises to enhance recovery.
→ Medications – Topical corticosteroids for inflammation, or vitamin A therapy in some cases.
→ Neurological care – Management of Parkinson’s or Alzheimer’s-related olfactory loss.
→ Avoiding triggers – Smoking cessation, reducing chemical exposure, or treating chronic sinus issues.
→ Supportive care – Safety measures for detecting hazards and improving dietary habits.
→ Psychological support – Counseling or therapy for anxiety or depression due to smell loss.
➤ Treatment Options in Korea
South Korea provides advanced ENT and neurological care for olfactory disorders:
Diagnosis in Korea
→ Nasal endoscopy and physical examination of nasal passages.
→ Olfactory function tests – Sniffin’ sticks, UPSIT (University of Pennsylvania Smell Identification Test).
→ Imaging: CT or MRI to evaluate sinus structures and brain regions.
→ Blood tests to identify infections, vitamin deficiencies, or systemic causes.
Medical Treatments in Korea
→ Topical or oral corticosteroids for inflammatory nasal disease.
→ Antibiotic therapy for bacterial sinusitis.
→ Antiviral treatments in selected viral infections.
→ Allergy management – Antihistamines, nasal sprays, or immunotherapy.
Advanced Therapies in Korea
→ Surgical interventions – Functional endoscopic sinus surgery (FESS) for polyps or chronic sinus obstruction.
→ Olfactory training programs under professional guidance.
→ Multidisciplinary care – ENT, neurology, and rehabilitation for chronic or neurological causes.
→ Integrative approaches – Korean traditional medicine techniques combined with Western therapy for supportive care.
Rehabilitation & Support in Korea
→ Education on smell recovery techniques and safety precautions.
→ Nutritional counseling to enhance flavor perception and maintain appetite.
→ Support for emotional well-being, coping strategies, and lifestyle adaptations.