Overview
Paroxysmal Nocturnal Dyspnea (PND) is a medical condition characterized by sudden episodes of severe shortness of breath that generally occur at night, waking a person from sleep. These episodes can be alarming and are often associated with underlying heart or lung problems. PND is distinct from general insomnia or nighttime discomfort, as it specifically involves respiratory distress. Individuals experiencing PND may feel a strong urge to sit up or stand to relieve the difficulty in breathing.
➤ PND is often linked to heart failure, where fluid accumulates in the lungs while lying down.
➤ Nighttime symptoms differentiate it from regular dyspnea, which can occur during the day or physical exertion.
➤ Immediate recognition is critical, as untreated PND may indicate worsening cardiac or pulmonary conditions.
PND is commonly observed in older adults, though it can appear in younger individuals with underlying heart conditions. Awareness of PND is essential for early diagnosis and effective management, particularly in healthcare systems like Korea, where specialized treatments and interventions are readily available.
Key Facts
➤ PND occurs primarily during sleep or nighttime rest.
➤ Patients usually awaken gasping for air, often after one to two hours of lying down.
➤ Commonly associated with left-sided heart failure, though other lung or systemic conditions can also trigger it.
➤ Relief is often found by sitting upright or standing, which decreases venous return and lung congestion.
➤ PND may be accompanied by cough, wheezing, or palpitations.
What is Paroxysmal Nocturnal Dyspnea?
Paroxysmal Nocturnal Dyspnea literally means “sudden shortness of breath at night.” It represents episodes where individuals suddenly awaken from sleep feeling intense breathlessness. The condition is typically a symptom rather than a standalone disease.
➤ Medical definition: PND is episodic and usually occurs 2–4 hours after falling asleep, often disrupting sleep quality.
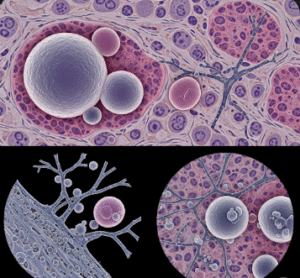
➤ Pathophysiology: While lying flat, gravity causes fluid from the lower extremities to shift toward the lungs, which can exacerbate pulmonary congestion.
➤ Distinction from orthopnea: Unlike simple orthopnea, which is shortness of breath while lying down, PND occurs after a latent period of sleep.
PND can significantly impact quality of life by disturbing sleep patterns, inducing anxiety, and affecting daily functioning.
What Symptoms Are Related To
PND often occurs alongside or signals other clinical symptoms, including:
➤ Orthopnea: Shortness of breath while lying flat.
➤ Fatigue: Persistent tiredness due to disrupted sleep.
➤ Peripheral edema: Swelling of ankles or legs, often indicating fluid retention.
➤ Cough or wheezing: Particularly when lying down.
➤ Palpitations: Awareness of irregular or rapid heartbeats.
➤ Nocturnal chest discomfort: In some cases, angina may accompany PND episodes.
Recognizing these associated symptoms helps clinicians identify underlying causes and severity, ensuring proper treatment.
What Causes / Possible Causes
PND is primarily caused by fluid accumulation in the lungs due to impaired heart or lung function. The main causes include:
➤ Left-sided heart failure: Most common cause; the heart fails to pump efficiently, leading to pulmonary congestion.
➤ Valvular heart diseases: Such as mitral stenosis or regurgitation, causing backflow and lung fluid accumulation.
➤ Cardiomyopathy: Weak or stiff heart muscle can precipitate fluid buildup.
➤ Chronic obstructive pulmonary disease (COPD) or asthma: Nighttime airway narrowing may trigger episodes.
➤ Sleep apnea: Obstructive sleep apnea can exacerbate breathing difficulties at night.
➤ Excessive fluid intake before bed or lying flat after meals may worsen symptoms in susceptible individuals.
Other systemic conditions, like kidney disease, may also contribute to fluid retention, indirectly increasing the risk of PND.
When Should I See My Doctor
PND is a warning sign of potentially serious heart or lung disease, so prompt medical attention is necessary.
➤ Immediate consultation is required if episodes are frequent, severe, or accompanied by chest pain, palpitations, or syncope.
➤ Seek help for recurring nighttime breathlessness, even if symptoms resolve after sitting upright.
➤ Monitoring related symptoms like swelling, fatigue, or daytime breathlessness is critical for early intervention.
➤ Medical evaluation should include ECG, echocardiogram, chest X-ray, and sometimes blood tests to assess heart function.
Ignoring PND may lead to progressive heart failure or worsening respiratory complications.
Care and Treatment
The treatment of PND focuses on addressing the underlying cause, alongside symptom management:
➤ Lifestyle modifications:
➤ Elevate the head while sleeping to reduce nighttime fluid accumulation.
➤ Limit salt intake to prevent fluid retention.
➤ Monitor daily weight to detect sudden fluid gain.
➤ Medications:
➤ Diuretics to reduce pulmonary congestion.
➤ ACE inhibitors or beta-blockers for managing heart failure.
➤ Bronchodilators or inhaled steroids if lung disease is involved.
➤ Monitoring and follow-up: Regular cardiac and pulmonary assessments help track improvement and prevent relapses.
➤ Emergency interventions: In acute episodes, sitting upright, using supplemental oxygen, or seeking immediate medical care is recommended.
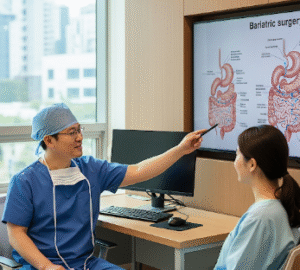
Treatment Options in Korea
Korea offers advanced medical facilities and specialized treatments for PND, particularly for heart-related causes:
➤ Cardiology centers in major hospitals provide comprehensive evaluation, including echocardiography, stress tests, and advanced imaging.
➤ Minimally invasive procedures such as valve repair or replacement for valvular disease are widely available.
➤ Heart failure management programs include medication optimization, lifestyle counseling, and remote monitoring.
➤ Pulmonology clinics offer specialized care for COPD, asthma, and sleep apnea with cutting-edge therapies.
➤ Integrative approaches such as Korean rehabilitation programs combine physical therapy, diet counseling, and personalized cardiac care.
➤ Patient support programs ensure long-term monitoring, education, and adherence to therapy.
Patients in Korea benefit from highly skilled specialists, modern hospital infrastructure, and structured follow-up, which significantly improve outcomes for PND.