Overview
A Marcus Gunn pupil, also known as a Relative Afferent Pupillary Defect (RAPD), is a clinical sign seen during an eye examination when there is an abnormal response of the pupils to light due to an issue with the optic nerve or severe retinal disease. Instead of constricting normally when light is shone into the affected eye, the pupil paradoxically dilates compared to the normal response.
This condition is not a disease itself but rather an important neurological and ophthalmological finding that helps doctors detect optic nerve damage, severe retinal disorders, or other underlying eye and brain conditions.
In Korea, Marcus Gunn pupil is carefully assessed by ophthalmologists and neurologists using specialized diagnostic equipment. Advanced facilities provide accurate detection and targeted treatment of the underlying cause, whether it is optic neuritis, glaucoma, or another eye disease.
Key Facts
➤ Marcus Gunn pupil = Relative Afferent Pupillary Defect (RAPD).
➤ Detected with the swinging flashlight test during an eye exam.
➤ Caused by damage to the optic nerve or severe retinal disease.
➤ Common in optic neuritis, glaucoma, retinal detachment, or ischemic optic neuropathy.
➤ In Korea, advanced ophthalmic centers provide early diagnosis using imaging and visual function tests.
What is Marcus Gunn Pupil?
A Marcus Gunn pupil is a neurological sign identified when light response in one eye is weaker than in the other. Normally, shining a light in one eye makes both pupils constrict equally (direct and consensual response). In Marcus Gunn pupil, when light is moved from the normal eye to the affected eye, the pupils paradoxically dilate instead of constricting. This occurs due to impaired transmission of light signals through the optic nerve or retina.
Symptoms Associated with Marcus Gunn Pupil
Marcus Gunn pupil itself is not felt by the patient but is observed by the doctor. However, patients may have related visual symptoms depending on the underlying condition:
➤ Blurred or reduced vision in one eye.
➤ Loss of color vision (optic neuritis).
➤ Visual field defects (glaucoma, retinal damage).
➤ Eye pain (commonly in optic neuritis, especially with eye movement).
➤ Sudden vision loss (ischemic optic neuropathy, retinal artery occlusion).
Causes / Possible Causes of Marcus Gunn Pupil
The sign develops due to asymmetrical damage to the optic nerve or retina. Common causes include:
Optic Nerve Causes
➤ Optic neuritis (often linked with multiple sclerosis).
➤ Ischemic optic neuropathy.
➤ Optic nerve compression from tumors.
➤ Glaucoma (advanced stage).
Retinal Causes
➤ Severe retinal detachment.
➤ Central retinal artery or vein occlusion.
➤ Macular degeneration (late stage).
When Should I See My Doctor?
You should seek medical help urgently if you notice vision problems such as:
➤ Sudden or severe vision loss in one eye.
➤ Eye pain with movement.
➤ Loss of color vision or contrast sensitivity.
➤ Visual field loss or patchy blind spots.
➤ Progressive worsening of sight despite glasses or treatment.
Because Marcus Gunn pupil often reflects a serious eye or neurological condition, timely diagnosis is essential.
Care and Treatment
Marcus Gunn pupil itself cannot be treated directly—it is a sign of an underlying condition. The focus is on diagnosing and managing the root cause:
➤ Optic neuritis → treated with corticosteroids and management of multiple sclerosis if present.
➤ Glaucoma → intraocular pressure control with medications, laser therapy, or surgery.
➤ Retinal detachment → urgent surgery (laser, cryotherapy, vitrectomy).
➤ Vascular occlusion → medical management and control of systemic conditions (diabetes, hypertension).
➤ Optic nerve compression → surgery or radiotherapy depending on the tumor.
Treatment Options in Korea
Korea is a leader in ophthalmology and neurology, offering cutting-edge diagnostic and treatment options for conditions associated with Marcus Gunn pupil.
Diagnosis
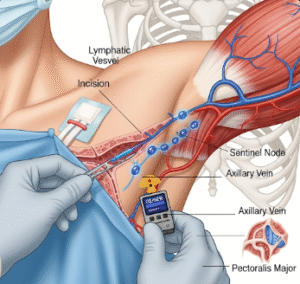
➤ Swinging flashlight test for RAPD detection.
➤ Optical Coherence Tomography (OCT) for retinal and optic nerve imaging.
➤ Visual field testing.
➤ MRI of the brain and orbits for suspected optic neuritis or tumors.
Medical & Surgical Treatments
➤ Corticosteroid therapy for optic neuritis.
➤ Advanced glaucoma surgeries (trabeculectomy, MIGS – minimally invasive glaucoma surgery).
➤ Retinal laser therapy and vitrectomy for detachment or vascular issues.
➤ Neuro-ophthalmology care for patients with multiple sclerosis or brain-related conditions.
Rehabilitation and Support
➤ Low-vision rehabilitation for patients with permanent sight loss.
➤ Long-term follow-up care for chronic diseases such as glaucoma or multiple sclerosis.