Overview
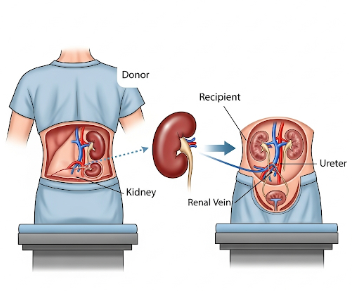
A living-donor transplant is a medical procedure where a healthy person donates an organ or a portion of an organ to someone in need of a transplant. Unlike deceased-donor transplants, this method allows patients to receive organs more quickly, often before their condition worsens. Living-donor transplants are commonly performed for kidneys and partial liver donations, but in certain cases, tissues like bone marrow, lung segments, or pancreas portions may also be donated.
Living donation provides hope for patients on long waiting lists, offering better survival rates and healthier organs since the donation is carefully planned.
What is a Living-Donor Transplant?
A living-donor transplant involves surgically removing an organ or part of an organ from a living, healthy person and implanting it into a recipient whose organ has failed. The donor can be a family member, a relative, or even an unrelated volunteer.
Common types of living-donor transplants:
- Kidney Transplant: Since people can live with one kidney, this is the most common type.
- Liver Transplant: A portion of the donor’s liver is removed; the liver has the unique ability to regenerate itself in both donor and recipient.
- Lung Transplant (rare): A lobe from two living donors can replace diseased lungs in a recipient.
- Pancreas and Intestine Segments: In highly selective cases.
- Bone Marrow / Stem Cell Donation: Healthy stem cells from a donor’s bone marrow or blood are given to the recipient.
Risks / Benefits
Benefits:
- Shorter waiting time compared to deceased-donor transplants.
- Healthier organs because surgery is planned in advance.
- Better survival rates and long-term outcomes for recipients.
- Emotional reward for donors, knowing they have saved or improved a life.
Risks for Recipients:
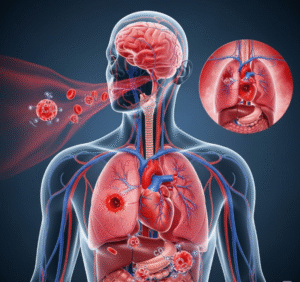
- Surgical complications (bleeding, infection, or organ rejection).
- Need for lifelong immunosuppressant medications.
- Possible complications if the organ does not function immediately.
Risks for Donors:
- Pain and recovery from surgery.
- Rare complications such as infection, blood clots, or organ failure.
- Emotional stress or anxiety.
How You Prepare
Preparation for a living-donor transplant involves both donor and recipient:
For the Donor:
- Comprehensive health evaluation including blood tests, imaging, psychological assessments, and lifestyle reviews.
- Tissue matching and compatibility testing with the recipient.
- Pre-surgery counseling to fully understand risks and benefits.
For the Recipient:
- Medical tests to confirm transplant eligibility.
- Stabilizing current health with medication and supportive care.
- Preparing mentally and emotionally for surgery and recovery.
- Making arrangements for post-surgery rehabilitation and support.
What You Can Expect
During the procedure:
- Donor surgery and recipient surgery are usually scheduled at the same time.
- The donor organ (or portion) is carefully removed by a surgical team.
- The organ is transplanted into the recipient immediately to ensure optimal function.
- Both donor and recipient are monitored in recovery units after the operation.
Surgery duration:
- Donor surgery typically takes 2–4 hours (kidney) or 6–8 hours (liver).
- Recipient surgery can last longer, depending on complexity.
After the Procedure
For the Donor:
- Hospital stay of a few days to a week, depending on the organ donated.
- Recovery time ranges from a few weeks (kidney) to several months (liver).
- Regular checkups to ensure long-term health.
For the Recipient:
- Longer hospital stay, often 1–3 weeks or more.
- Immunosuppressant medications are prescribed to prevent organ rejection.
- Frequent medical monitoring including blood tests and imaging.
- Risk of infection requires strict hygiene and dietary precautions.
Results
- Recipient outcomes: Living-donor transplants generally have higher success rates than deceased-donor transplants. Kidney transplants from living donors can last 15–20 years, while liver grafts can function for decades.
- Donor outcomes: Most donors return to normal health and lifestyle after recovery, with no long-term health problems if carefully selected.
- Psychological impact: Both donors and recipients often report improved emotional well-being, though ongoing support may be needed.
Life After a Living-Donor Transplant
For Donors:
- Most donors lead normal, healthy lives after recovery.
- Lifestyle changes such as a balanced diet, exercise, and avoiding smoking or heavy drinking support long-term health.
- Regular medical follow-up is recommended.
For Recipients:
- Lifelong commitment to immunosuppressant therapy.
- Careful monitoring for signs of rejection or infection.
- Healthy lifestyle practices, including exercise, nutrition, and stress management.
- Emotional adjustments as they adapt to living with a new organ.
Long-term outlook:
Many patients return to work, enjoy family life, and regain independence. Donors often continue their lives without limitations while taking pride in having transformed another person’s future.