Overview
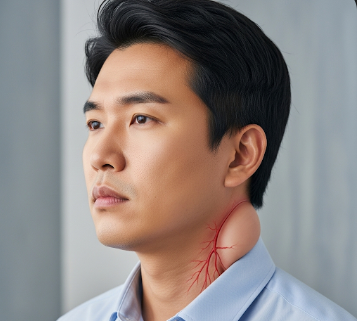
Jugular vein distention (JVD) is a clinical sign where the jugular veins in the neck appear visibly swollen or enlarged. It is often a symptom of underlying cardiovascular or systemic conditions, rather than a disease itself. JVD can indicate elevated central venous pressure, which is commonly associated with heart failure, fluid overload, or venous obstruction.
In Korea, cardiology clinics and hospitals provide advanced diagnostic and treatment options for patients presenting with JVD, combining imaging, laboratory tests, and therapeutic interventions to manage the underlying cause effectively. Early recognition is crucial to prevent complications and optimize heart function.
Key Facts
- ➔ JVD is most commonly observed in conditions causing elevated right atrial pressure.
- ➔ It is a visible bulging of the neck veins, particularly when the patient is sitting at a 45-degree angle.
- ➔ Causes include heart failure, pericardial effusion, tricuspid valve disease, pulmonary hypertension, and superior vena cava obstruction.
- ➔ JVD may be accompanied by other symptoms such as shortness of breath, edema, or fatigue.
- ➔ Prompt evaluation and treatment of the underlying cause can improve outcomes and prevent complications.
What is Jugular Vein Distention?
Jugular vein distention is the visible enlargement of the external jugular or internal jugular veins in the neck, often reflecting elevated central venous pressure.
- ➔ Mechanism: Increased pressure in the right atrium or superior vena cava is transmitted to the jugular veins, causing them to bulge.
- ➔ Assessment: Clinicians observe the neck veins while the patient is reclining at a 30–45° angle, measuring the height of venous distention.
- ➔ Clinical significance: JVD serves as an important non-invasive indicator of heart function and fluid status.
- ➔ Related conditions: May be seen in acute or chronic heart failure, cardiac tamponade, constrictive pericarditis, or pulmonary hypertension.
Recognizing JVD during a physical examination can provide critical insights into cardiovascular health.
What Symptoms Are Related To
JVD itself is a sign rather than a symptom, but it often occurs alongside:
- ➔ Swelling in the legs, ankles, or abdomen (edema)
- ➔ Shortness of breath or difficulty breathing, especially when lying down
- ➔ Fatigue or weakness
- ➔ Rapid or irregular heartbeat (palpitations)
- ➔ Weight gain due to fluid retention
- ➔ Coughing or wheezing
- ➔ Chest pain in cases related to heart conditions
Monitoring associated symptoms helps identify the severity and underlying cause of JVD.
What Causes / Possible Causes
JVD can result from cardiovascular, pulmonary, or systemic disorders:
- ➔ Heart failure: Right-sided or biventricular failure increases venous pressure.
- ➔ Constrictive pericarditis: Thickened pericardium limits heart filling, raising venous pressure.
- ➔ Cardiac tamponade: Fluid accumulation in the pericardium compresses the heart, elevating jugular pressure.
- ➔ Tricuspid valve disease: Regurgitation or stenosis leads to backflow and venous congestion.
- ➔ Pulmonary hypertension: Increased pulmonary artery pressure strains the right heart.
- ➔ Superior vena cava obstruction: Tumors or thrombus can block venous return.
- ➔ Fluid overload: Excess intravenous fluids or kidney failure may contribute to venous distention.
Accurate identification of the underlying cause is critical for effective management.
When Should I See My Doctor
Medical evaluation is warranted if you notice:
- ➔ Persistent or prominent swelling of neck veins
- ➔ Shortness of breath, fatigue, or palpitations
- ➔ Leg, ankle, or abdominal swelling
- ➔ Chest pain or pressure
- ➔ Rapid weight gain due to fluid retention
- ➔ History of heart disease, kidney disease, or pulmonary hypertension
Prompt consultation ensures early diagnosis and treatment, reducing the risk of heart failure or other complications.
Care and Treatment
Management of JVD focuses on treating the underlying condition and alleviating symptoms:
- ➔ Lifestyle modifications: Limiting salt intake, managing fluid balance, and regular monitoring of weight.
- ➔ Medication: Diuretics to reduce fluid overload, ACE inhibitors, beta-blockers, or vasodilators for heart conditions.
- ➔ Treatment of underlying cardiac disorders: Correcting valvular disease, pericardial effusion, or pulmonary hypertension.
- ➔ Procedures: Pericardiocentesis for cardiac tamponade, or surgical intervention for obstructed veins.
- ➔ Monitoring: Regular follow-up with echocardiography, blood tests, and clinical examination to assess fluid status.
- ➔ Hospitalization: Required for acute decompensated heart failure or severe fluid overload.
Timely treatment of the underlying cause often leads to resolution of JVD and improvement in associated symptoms.
Treatment Options in Korea
Korean cardiology and internal medicine centers provide comprehensive care for patients with JVD:
- ➔ Clinical assessment: Detailed physical examination, including JVD measurement, and history of cardiovascular risk factors.
- ➔ Diagnostic imaging: Echocardiography, chest X-ray, CT, or MRI to assess heart function and venous structures.
- ➔ Laboratory testing: Blood tests including BNP/NT-proBNP for heart failure assessment, kidney function, and electrolytes.
- ➔ Medical therapy: Diuretics, vasodilators, inotropes, or disease-specific medications.
- ➔ Minimally invasive procedures: Pericardiocentesis, catheter-based interventions for venous obstruction, or pacemaker placement if indicated.
- ➔ Multidisciplinary care: Collaboration between cardiology, nephrology, and pulmonology specialists for optimal management.
Top hospitals such as Seoul National University Hospital, Asan Medical Center, and Samsung Medical Center offer advanced diagnostic tools and individualized treatment plans to ensure effective management of JVD and associated cardiovascular conditions.
In Summary: Jugular vein distention is a visible marker of elevated central venous pressure, often associated with heart or systemic disorders. Early recognition, accurate diagnosis, and specialized treatment in Korea can improve cardiovascular function, reduce symptoms, and prevent life-threatening complications.
- ➔ Key Takeaway: Persistent or prominent JVD requires prompt evaluation to identify and manage underlying causes.
- ➔ Action Point: Consult a cardiologist for comprehensive assessment and personalized treatment strategies.