Overview
Eye (intraocular) pressure (IOP) refers to the fluid pressure inside the eye, which is essential for maintaining the eye’s shape, structural integrity, and proper functioning. Normal intraocular pressure helps the eye maintain its optical properties and protects internal structures, including the retina and optic nerve. Elevated or reduced IOP can indicate ocular health issues, most notably glaucoma, which is a leading cause of irreversible blindness worldwide. In Korea, ophthalmology clinics and specialized eye centers offer comprehensive IOP measurement, monitoring, and treatment options to protect vision and manage ocular disorders.
Highlights:
➤ Pressure within the eye maintaining shape and function – Critical for healthy vision
➤ Imbalance may lead to glaucoma or optic nerve damage
➤ Regular monitoring is essential for early detection of eye disease
Key Facts
➤ Normal IOP range: Typically 10–21 mmHg; variations depend on measurement technique and individual factors
➤ Prevalence: Elevated IOP is a primary risk factor for glaucoma; millions worldwide are affected
➤ Age affected: Risk increases with age, but can occur in young adults or children in certain conditions
➤ Gender: Both males and females are affected; some studies suggest slight age-related gender differences
➤ Impact: Elevated IOP may cause optic nerve damage, vision loss, or glaucoma, whereas abnormally low IOP can indicate ocular hypotony or trauma
What is Eye (Intraocular) Pressure?
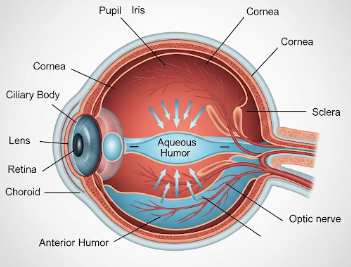
Intraocular pressure is the force exerted by aqueous humor (the fluid inside the eye) against the walls of the eyeball. Proper IOP results from a balance between aqueous humor production and drainage. Key points include:
- Aqueous humor production: Secreted by the ciliary body to nourish ocular tissues
- Drainage: Occurs via the trabecular meshwork and uveoscleral pathways
- Balance: Normal eye function requires production and drainage to be in equilibrium
Highlights:
➤ Maintains eye shape and optical properties
➤ Protects delicate structures like the retina and optic nerve
➤ Imbalance can lead to ocular disease
What Symptoms Are Related to Abnormal IOP?
➤ Often asymptomatic in early stages – Especially in chronic glaucoma
➤ Eye pain or pressure – May occur in acute angle-closure glaucoma
➤ Blurred vision or halos around lights – Common in sudden IOP spikes
➤ Headaches – Usually frontal or around the eyes
➤ Nausea and vomiting – Rare, associated with acute angle-closure
➤ Peripheral vision loss – Gradual in chronic elevated IOP
➤ Redness of the eye – May accompany acute IOP elevation
Highlights:
➣ Early IOP abnormalities often do not produce noticeable symptoms, making routine checks critical
➣ Sudden changes in IOP require immediate ophthalmologic evaluation
What Causes / Possible Causes
➤ Primary open-angle glaucoma: Gradual blockage of aqueous drainage leading to increased IOP
➤ Angle-closure glaucoma: Sudden blockage of drainage angle causing rapid IOP rise
➤ Ocular trauma: Injuries can disrupt aqueous flow or damage the eye
➤ Eye surgery or inflammation: Post-surgical changes or uveitis may alter IOP
➤ Medications: Corticosteroids can elevate intraocular pressure in susceptible individuals
➤ Systemic conditions: Diabetes, hypertension, and thyroid disorders may indirectly affect IOP
Highlights:
➣ Causes range from chronic degenerative conditions to acute emergencies
➣ Identifying the underlying cause is crucial for preventing vision loss
When Should I See My Doctor?
➤ Routine eye examinations: Regular IOP checks for adults over 40 or at-risk individuals
➤ Sudden eye pain or vision changes – Possible acute glaucoma
➤ Family history of glaucoma – Increases risk of elevated IOP
➤ Redness, halos, or headaches with visual symptoms – Requires urgent assessment
➤ Post-surgery or eye trauma – Monitoring for secondary IOP elevation
Highlights:
➣ Early consultation at a Korean ophthalmology clinic can prevent irreversible optic nerve damage
➣ Timely intervention is key to preserving vision
Care and Treatment
➤ Medications: Topical eye drops (prostaglandin analogs, beta-blockers, carbonic anhydrase inhibitors) to lower IOP
➤ Laser therapy: Laser trabeculoplasty or iridotomy to improve aqueous outflow
➤ Surgical interventions: Trabeculectomy or minimally invasive glaucoma surgery for refractory cases
➤ Lifestyle and monitoring: Avoiding excessive caffeine, maintaining cardiovascular health, and regular IOP checks
➤ Follow-up care: Continuous monitoring to prevent progression of glaucoma or optic nerve damage
Highlights:
➣ Treatment aims to lower IOP, prevent optic nerve damage, and maintain vision
➣ Personalized plans depend on severity, type of glaucoma, and patient factors
Treatment Options in Korea
Medical Treatments:
➤ Ophthalmology clinics: Comprehensive eye exams, tonometry, and optic nerve assessment
➤ Pharmacological therapy: Prescription eye drops to manage elevated IOP
➤ Laser treatments: Non-invasive procedures for angle-closure or open-angle glaucoma
Advanced Procedures:
➤ Trabeculectomy and glaucoma drainage devices: Surgical options for uncontrolled IOP
➤ Minimally invasive glaucoma surgeries (MIGS): Modern techniques for safer pressure reduction
➤ Imaging and monitoring: Optical coherence tomography (OCT) to track optic nerve health
Rehabilitation & Follow-Up Care:
➤ Regular IOP measurements and optic nerve evaluations
➤ Education on medication adherence and symptom monitoring
➤ Multidisciplinary support for vision preservation and lifestyle management
Highlights:
➣ Korean eye centers provide state-of-the-art diagnostics, treatment, and long-term monitoring
➣ Early detection and management improve visual outcomes and quality of life