Overview
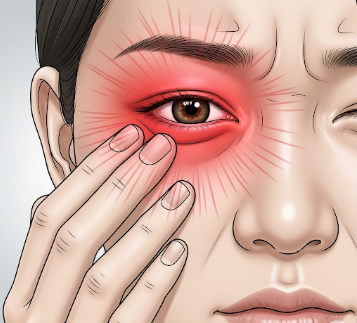
Eye pain refers to any discomfort, soreness, or aching sensation in or around the eyes. It can range from mild irritation to severe, debilitating pain and may be sudden or gradual in onset. Eye pain is often associated with other symptoms such as redness, blurred vision, tearing, or light sensitivity, and can indicate a wide variety of conditions, including infections, inflammation, trauma, or systemic diseases. In Korea, ophthalmology clinics and specialized eye centers provide comprehensive assessment, diagnosis, and treatment for eye pain, ensuring both symptom relief and protection of vision.
Highlights:
➤ Discomfort or soreness in or around the eye – Can be mild or severe
➤ Associated with multiple ocular and systemic conditions
➤ Requires careful evaluation to prevent vision-threatening complications
Key Facts
➤ Prevalence: Eye pain is a common complaint across all age groups
➤ Age affected: Can affect children, adults, and the elderly
➤ Gender: Both males and females are equally affected
➤ Impact: May interfere with daily activities, reading, computer work, or driving
➤ Urgency: Sudden, severe, or unilateral eye pain may indicate an emergency condition such as acute glaucoma or optic neuritis
What is Eye Pain?
Eye pain is defined as any sensation of discomfort, ache, or sharp pain in or around the eyeball. It may be classified as:
- Anterior eye pain: Involving the cornea, conjunctiva, or anterior segment
- Posterior eye pain: Deep, retro-orbital pain, often linked to optic nerve or orbital structures
- Referred pain: From sinus infections, dental problems, or neurological causes
Key characteristics include:
- Sharp, throbbing, or aching sensation
- Localized or diffuse across one or both eyes
- May worsen with eye movement, light exposure, or blinking
Highlights:
➤ Variety of causes require careful evaluation
➤ Can be acute or chronic
➤ May be accompanied by visual changes or systemic symptoms
What Symptoms Are Related to Eye Pain?
➤ Redness of the eye – Common in infections, inflammation, or trauma
➤ Tearing or watery eyes – Reflex response to irritation or dryness
➤ Blurred vision or visual disturbances – Often associated with corneal, retinal, or optic nerve involvement
➤ Sensitivity to light (photophobia) – Indicates anterior segment inflammation or neurological issues
➤ Swelling around the eye – May occur in infections or orbital conditions
➤ Headache – Often accompanies eye pain in migraine, glaucoma, or sinusitis
➤ Foreign body sensation – Feeling of grit or debris in the eye
Highlights:
➣ Symptoms vary depending on underlying cause and severity
➣ Persistent or severe pain warrants prompt ophthalmologic evaluation
What Causes / Possible Causes
➤ Corneal abrasions or ulcers: Trauma, contact lens use, or infections
➤ Conjunctivitis: Viral, bacterial, or allergic inflammation
➤ Uveitis or iritis: Inflammation of the uveal tract
➤ Glaucoma: Acute angle-closure glaucoma causes sudden, severe pain
➤ Optic neuritis: Inflammation of the optic nerve causing deep retro-orbital pain
➤ Sinus infections: Can cause referred pain behind the eye
➤ Trauma: Blunt or penetrating eye injuries
➤ Foreign bodies: Dust, metal, or chemical exposure
➤ Systemic diseases: Migraines, giant cell arteritis, or autoimmune conditions
Highlights:
➣ Eye pain may originate from ocular, orbital, systemic, or neurological causes
➣ Correct diagnosis is crucial to prevent vision loss and manage systemic conditions
When Should I See My Doctor?
➤ Sudden or severe eye pain – Especially with redness or visual changes
➤ Accompanied by vision loss, halos, or flashes of light – Could indicate glaucoma or retinal issues
➤ History of trauma or foreign body – Immediate evaluation required
➤ Persistent pain without obvious cause – To rule out infections or inflammatory diseases
➤ Associated neurological symptoms – Such as headache, facial pain, or weakness
Highlights:
➣ Early evaluation at a Korean ophthalmology clinic ensures correct diagnosis
➣ Timely management prevents complications and preserves vision
Care and Treatment
➤ Artificial tears or lubricating drops: For dryness-induced pain
➤ Topical antibiotics or antivirals: For infections
➤ Anti-inflammatory medications: Steroid or non-steroidal eye drops for uveitis or other inflammation
➤ Pain relief: Analgesics for mild discomfort, under medical guidance
➤ Removal of foreign bodies: By trained ophthalmologist
➤ Surgical interventions: For severe glaucoma, corneal ulcers, or trauma
➤ Lifestyle adjustments: Avoiding eye strain, taking breaks from screens, proper contact lens hygiene
Highlights:
➣ Treatment is cause-specific
➣ Combines symptom relief, infection control, and preventive measures
Treatment Options in Korea
Medical Treatments:
➤ Ophthalmology clinics: Comprehensive eye exams, corneal evaluation, and tonometry
➤ Prescription medications: Antibiotics, antivirals, or anti-inflammatory drops
➤ Artificial tears and lubricants: Customized for dry eye or irritative conditions
Advanced Procedures:
➤ Laser or surgical interventions: For glaucoma, corneal ulcers, or severe trauma
➤ Orbital imaging: CT or MRI for orbital or neurological causes
➤ Follow-up care: Monitoring for chronic conditions and response to therapy
Rehabilitation & Follow-Up Care:
➤ Education on preventive strategies, proper lens care, and visual ergonomics
➤ Regular check-ups for high-risk patients or chronic ocular conditions
➤ Multidisciplinary support for patients with systemic diseases affecting eye health
Highlights:
➣ Korean eye centers provide advanced diagnostics, tailored treatments, and continuous follow-up
➣ Early intervention ensures symptom relief, prevention of complications, and vision preservation