Overview
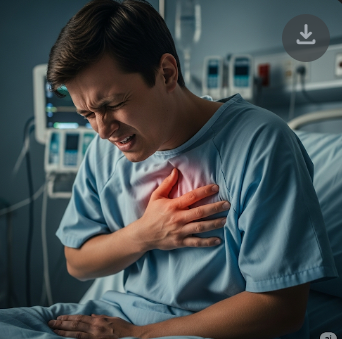
Chest pain is a common symptom that can arise from a variety of conditions affecting the heart, lungs, digestive system, muscles, or nerves. It can range from mild discomfort to severe, life-threatening pain, making timely evaluation essential. In Korea, hospitals provide comprehensive diagnostics, advanced imaging, and multidisciplinary treatment for chest pain, ensuring accurate identification of causes and prompt management to prevent complications.
Key Facts
▶ Prevalence: Chest pain affects people of all ages, with higher risk in older adults and those with cardiovascular disease.
▶ Causes: Heart attack, angina, pulmonary embolism, pneumonia, acid reflux, muscle strain, or anxiety.
▶ Associated Symptoms: Shortness of breath, dizziness, palpitations, nausea, sweating, or radiating pain.
▶ Treatment Options in Korea: Cardiology, pulmonology, gastroenterology, and pain management interventions.
▶ Urgency: Sudden or severe chest pain may indicate a medical emergency, requiring immediate care.
What is Chest Pain?
Chest pain is any discomfort, pressure, or tightness in the chest area, which may originate from the heart, lungs, gastrointestinal tract, muscles, or nerves.
▶ Cardiac Chest Pain: Often caused by reduced blood flow to the heart (angina) or heart attack (myocardial infarction).
▶ Pulmonary Chest Pain: Resulting from lung infections, pulmonary embolism, or pleuritis.
▶ Gastrointestinal Chest Pain: Acid reflux, gastritis, or esophageal spasms can mimic heart-related pain.
▶ Musculoskeletal Chest Pain: Muscle strain, rib injury, or inflammation of cartilage.
▶ Psychogenic Chest Pain: Anxiety, panic attacks, or stress-related episodes.
Note: Identifying the source of chest pain is critical because cardiac causes can be life-threatening.
What Symptoms Are Related to Chest Pain?
▶ Pressure or Tightness: Often described as squeezing or heaviness in the chest.
▶ Sharp or Stabbing Pain: May occur with lung or muscle-related causes.
▶ Radiating Pain: To the arm, neck, jaw, or back, often associated with heart problems.
▶ Shortness of Breath: Difficulty breathing can accompany cardiac or pulmonary causes.
▶ Palpitations: Rapid or irregular heartbeat alongside pain.
▶ Sweating or Nausea: Common in heart attacks.
▶ Dizziness or Fainting: May indicate severe cardiovascular compromise.
▶ Persistent or Intermittent Pain: Depending on underlying cause, pain may fluctuate or persist.
What Causes / Possible Causes
Chest pain arises from multiple body systems, each with distinct mechanisms:
▶ Cardiovascular Causes: Heart attack, angina, pericarditis, aortic dissection.
▶ Respiratory Causes: Pulmonary embolism, pneumonia, pleuritis, or pneumothorax.
▶ Gastrointestinal Causes: Acid reflux (GERD), esophageal spasms, peptic ulcers.
▶ Musculoskeletal Causes: Rib fractures, muscle strain, costochondritis.
▶ Psychological Causes: Panic attacks, anxiety disorders, or stress-related symptoms.
▶ Other Causes: Shingles (herpes zoster) or referred pain from neck or abdomen.
Note: Sudden, severe, or radiating chest pain should be treated as a medical emergency until proven otherwise.
When Should I See a Doctor?
▶ Sudden Severe Chest Pain: Especially if associated with sweating, nausea, or shortness of breath.
▶ Persistent Chest Pain: Lasting more than a few minutes or recurring frequently.
▶ Radiating Pain: To arm, neck, jaw, or back.
▶ Associated Symptoms: Dizziness, palpitations, fainting, or shortness of breath.
▶ High-Risk Individuals: Older adults, smokers, those with high blood pressure, diabetes, or family history of heart disease.
▶ Post-Trauma Pain: Following injury to chest or ribcage.
▶ Children or Elderly: Prompt evaluation is crucial to rule out serious conditions.
▶ Lifestyle-Related Pain: Pain associated with heavy exertion or stress.
Tip: In Korea, cardiologists, pulmonologists, gastroenterologists, and emergency specialists provide comprehensive evaluation to determine the exact cause of chest pain.
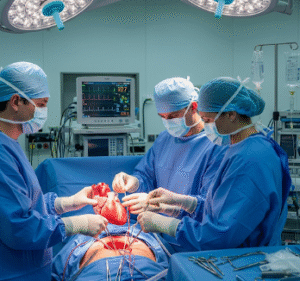
Care and Treatment
Treatment depends on cause, severity, and underlying risk factors:
▶ Cardiac Causes: Immediate interventions, including medications, angioplasty, or surgery for heart attacks or angina.
▶ Pulmonary Causes: Antibiotics for infections, anticoagulants for pulmonary embolism, or supportive therapy for pleuritis.
▶ Gastrointestinal Causes: Proton pump inhibitors, dietary modifications, or treatment of esophageal disorders.
▶ Musculoskeletal Causes: Pain relief, physical therapy, or anti-inflammatory medications.
▶ Psychogenic Causes: Counseling, stress management, or medications for anxiety.
▶ Lifestyle Modifications: Smoking cessation, regular exercise, healthy diet, and stress management.
▶ Monitoring: Regular follow-ups for chronic conditions or recurrent chest pain.
Treatment Options in Korea
Medical Evaluation:
▶ Cardiology Assessment: ECG, echocardiography, stress tests, and cardiac enzymes.
▶ Pulmonology Evaluation: Chest X-ray, CT scan, and pulmonary function tests.
▶ Gastroenterology Assessment: Endoscopy, pH monitoring, or esophageal motility studies.
▶ Laboratory Tests: Blood tests, lipid profile, and inflammatory markers.
▶ Emergency Care: Immediate interventions in severe cases, including angioplasty or thrombolysis.
Advanced Therapies:
▶ Interventional Procedures: Angioplasty, stent placement, or pacemaker insertion for cardiac causes.
▶ Pulmonary Interventions: Bronchoscopy, pulmonary embolism treatment, or respiratory therapy.
▶ Surgical Options: For trauma, tumors, or severe gastrointestinal complications.
▶ Integrated Multidisciplinary Care: Coordination among cardiology, pulmonology, gastroenterology, and pain specialists.
Rehabilitation & Support:
▶ Patient Education: Guidance on recognizing warning signs, lifestyle modifications, and medication adherence.
▶ Follow-Up Care: Monitoring treatment effectiveness and preventing recurrence.
▶ Specialist Clinics: Korean hospitals provide comprehensive clinics integrating cardiology, pulmonology, gastroenterology, and rehabilitation services.
Outcome: With prompt evaluation and treatment in Korea, chest pain can be managed effectively, ensuring patient safety, reducing risk of serious complications, and improving overall quality of life.