Overview
Blood in stool, medically referred to as hematochezia (bright red blood) or melena (black, tarry stools), is a concerning symptom that indicates bleeding somewhere in the gastrointestinal (GI) tract. The color, consistency, and frequency of blood can help determine the source of bleeding, ranging from minor conditions such as hemorrhoids to more serious gastrointestinal diseases including ulcers, inflammatory bowel disease, or colorectal cancer. In Korea, hospitals and gastroenterology clinics offer advanced diagnostic evaluations, endoscopic procedures, and targeted treatments to identify and manage the underlying causes of blood in stool effectively.
Key Facts
▶ Prevalence: Blood in stool is relatively common and can occur in both adults and children.
▶ Appearance: Bright red, dark red, or black, tarry stools depending on the bleeding site.
▶ Causes: Hemorrhoids, anal fissures, gastrointestinal infections, ulcers, polyps, or cancers.
▶ Associated Symptoms: Abdominal pain, diarrhea, constipation, weakness, or anemia.
▶ Treatment Options in Korea: Endoscopic therapy, medication, surgery, lifestyle and dietary interventions.
What is Blood in Stool?
Blood in stool occurs when bleeding takes place in the gastrointestinal tract, from the esophagus to the rectum.
▶ Hematochezia: Bright red blood, usually from the lower GI tract (rectum or colon).
▶ Melena: Black, tarry stools, often from upper GI bleeding (stomach or small intestine).
▶ Occult Bleeding: Small amounts of blood not visible to the naked eye, detected via stool tests.
Note: The type, color, and amount of blood help physicians determine the source and severity of bleeding.
What Symptoms Are Related to Blood in Stool?
▶ Visible Blood: Bright red streaks or black, tarry stools.
▶ Abdominal Pain: Cramping, bloating, or localized discomfort.
▶ Changes in Bowel Habits: Diarrhea, constipation, or alternating bowel patterns.
▶ Weakness or Fatigue: Resulting from blood loss and anemia.
▶ Dizziness or Lightheadedness: Especially with significant bleeding.
▶ Nausea or Vomiting: Sometimes accompanying gastrointestinal bleeding.
▶ Unexplained Weight Loss: In chronic or severe cases.
▶ Fever or Signs of Infection: May indicate infectious causes.
What Causes / Possible Causes
Blood in stool can result from various gastrointestinal, systemic, or structural factors:
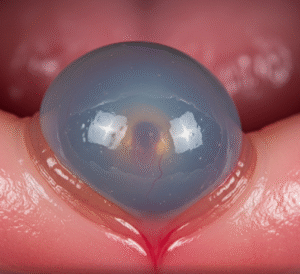
▶ Hemorrhoids: Swollen veins in the rectum or anus causing bleeding during defecation.
▶ Anal Fissures: Small tears in the anal lining due to constipation or trauma.
▶ Gastrointestinal Infections: Bacterial, viral, or parasitic infections causing inflammation and bleeding.
▶ Peptic Ulcers: Open sores in the stomach or duodenum leading to upper GI bleeding.
▶ Inflammatory Bowel Disease (IBD): Crohn’s disease or ulcerative colitis causing chronic intestinal bleeding.
▶ Polyps or Tumors: Benign or malignant growths in the colon or rectum.
▶ Diverticulosis: Small pouches in the colon wall that can bleed.
▶ Medication Effects: NSAIDs, anticoagulants, or certain antibiotics increasing bleeding risk.
▶ Vascular Malformations: Abnormal blood vessels in the GI tract.
Note: Identifying the exact cause requires medical evaluation, imaging, and sometimes endoscopic procedures.
When Should I See a Doctor?
▶ Persistent or Recurrent Bleeding: Continuous presence of blood in stool over days or weeks.
▶ Severe Bleeding: Large amounts of blood causing dizziness, weakness, or anemia.
▶ Associated Pain or Cramping: Significant abdominal discomfort with bleeding.
▶ Unexplained Weight Loss or Fatigue: May indicate chronic or serious underlying disease.
▶ Family History: Colorectal cancer or gastrointestinal disorders.
▶ Changes in Stool Patterns: New-onset constipation, diarrhea, or alternating bowel habits.
▶ Other Symptoms: Fever, vomiting blood, or black, tarry stools requiring urgent attention.
Tip: Prompt evaluation helps detect serious conditions early, ensuring timely treatment and better outcomes.
Care and Treatment
Management depends on the cause, location, and severity of bleeding:
▶ Hemorrhoid and Fissure Care: Topical ointments, sitz baths, and dietary fiber to ease bowel movements.
▶ Medication Management: Proton pump inhibitors for ulcers, antibiotics for infections, or anti-inflammatory drugs for IBD.
▶ Dietary Adjustments: High-fiber diet, adequate hydration, and avoidance of irritant foods.
▶ Monitoring: Regular stool checks, blood tests for anemia, and symptom tracking.
▶ Lifestyle Measures: Reducing straining during defecation, regular exercise, and managing stress.
▶ Surgical or Endoscopic Interventions: Polyp removal, ulcer treatment, or repair of structural abnormalities as needed.
Treatment Options in Korea
Medical Evaluation:
▶ Gastroenterology Consultation: Comprehensive examination including medical history, physical exam, and risk assessment.
▶ Laboratory Tests: Complete blood count, stool analysis, and tests for infection or inflammation.
▶ Endoscopy: Colonoscopy or upper GI endoscopy to locate bleeding sources.
▶ Imaging: CT scan or MRI if structural abnormalities are suspected.
Advanced Therapies:
▶ Endoscopic Hemostasis: Treats bleeding ulcers, polyps, or vascular lesions.
▶ Surgical Intervention: For severe bleeding, tumors, or refractory gastrointestinal conditions.
▶ Medication Therapy: Proton pump inhibitors, anti-inflammatory drugs, or antibiotics depending on the cause.
▶ Blood Transfusions: For significant anemia resulting from chronic or acute blood loss.
Rehabilitation & Support:
▶ Patient Education: Recognizing symptoms, maintaining bowel health, and adhering to treatment plans.
▶ Follow-Up Care: Monitoring for recurrence and managing chronic gastrointestinal disorders.
▶ Specialist Clinics: Korean hospitals provide integrated care combining gastroenterology, surgery, nutrition, and patient education.
Outcome: With timely evaluation and comprehensive treatment in Korea, most cases of blood in stool are effectively managed, reducing complications, promoting gastrointestinal health, and improving quality of life.