Overview
Blackouts, medically referred to as syncope or temporary loss of consciousness, are episodes where an individual suddenly becomes unresponsive and may collapse. These events are usually brief, lasting seconds to a few minutes, and can occur due to insufficient blood flow or oxygen to the brain. While some blackouts are benign, others may signal underlying heart, neurological, or metabolic disorders. In Korea, hospitals and specialized clinics provide comprehensive evaluation, diagnosis, and treatment for blackouts, combining advanced cardiac, neurological, and metabolic assessments with preventive care.
Key Facts
▶ Prevalence: Fainting or blackouts affect people of all ages, with higher incidence among the elderly.
▶ Common Triggers: Dehydration, prolonged standing, sudden position changes, stress, or medical conditions.
▶ Associated Risks: Falls and injuries during an episode, underlying heart or neurological issues.
▶ Causes: Cardiovascular, neurological, metabolic, or situational triggers.
▶ Treatment Options in Korea: Medical evaluation, diagnostic tests, medication, lifestyle interventions, and rehabilitation programs.
What is a Blackout?
A blackout is a temporary episode of loss of consciousness, usually preceded by warning signs such as dizziness, lightheadedness, or visual disturbances. The underlying mechanism often involves reduced blood flow or oxygen supply to the brain.
▶ Syncope: Brief loss of consciousness with rapid recovery.
▶ Fainting: Common form of blackout, often triggered by stress, standing, or pain.
▶ Seizure-related Loss of Consciousness: Distinguished from fainting by convulsions, prolonged post-episode confusion, or tongue biting.
Note: Accurate diagnosis is essential to distinguish benign blackouts from life-threatening causes like cardiac arrhythmias or neurological disorders.
What Symptoms Are Related to Blackouts?
▶ Dizziness or Lightheadedness: Often preceding a blackout.
▶ Visual Disturbances: Blurred vision, tunnel vision, or “spots” before loss of consciousness.
▶ Nausea or Sweating: Common warning signs.
▶ Palpitations or Rapid Heartbeat: May indicate a cardiac cause.
▶ Confusion After Episode: Temporary disorientation post-blackout.
▶ Falling or Injury: Potential risk during the loss of consciousness.
▶ Pale or Clammy Skin: Common physical manifestation.
What Causes / Possible Causes
Blackouts can result from various cardiovascular, neurological, metabolic, or situational factors:
▶ Cardiovascular Causes: Arrhythmias, heart block, heart valve disease, or heart attack.
▶ Neurally Mediated Syncope: Fainting due to sudden stress, pain, or standing too long.
▶ Orthostatic Hypotension: Drop in blood pressure upon standing.
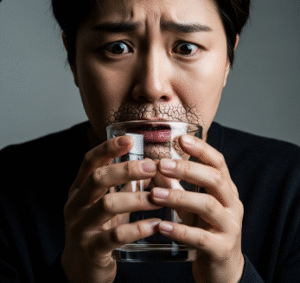
▶ Dehydration or Electrolyte Imbalance: Reduced blood volume leading to cerebral hypoperfusion.
▶ Neurological Causes: Seizures, migraines, or transient ischemic attacks (TIAs).
▶ Metabolic Causes: Hypoglycemia, anemia, or low oxygen levels.
▶ Medications: Blood pressure medications, diuretics, or sedatives.
▶ Environmental Factors: Heat exposure, overcrowding, or sudden exertion.
Note: Age, frequency of blackouts, and associated symptoms help determine the urgency and type of evaluation required.
When Should I See a Doctor?
▶ Frequent or Recurrent Blackouts: Occurring multiple times or without clear triggers.
▶ Associated Chest Pain or Palpitations: Possible cardiac involvement.
▶ Neurological Symptoms: Seizures, weakness, numbness, or speech difficulties.
▶ Injury During Blackout: Falls causing trauma or fractures.
▶ Post-Blackout Confusion: Prolonged disorientation or unusual behavior.
▶ Underlying Conditions: Heart disease, diabetes, or neurological disorders.
Tip: Even a single unexplained blackout warrants medical evaluation to rule out serious causes and prevent complications.
Care and Treatment
Management depends on the underlying cause and risk factors:
▶ Immediate Care: Lay the person down, elevate legs, and ensure a safe environment during an episode.
▶ Hydration and Nutrition: Maintaining adequate fluid and electrolyte balance.
▶ Medication Adjustment: Reviewing medications that may contribute to low blood pressure or heart rhythm disturbances.
▶ Lifestyle Measures: Avoiding prolonged standing, sudden postural changes, or overheating.
▶ Monitoring: Keeping a record of blackout episodes, triggers, and symptoms for medical evaluation.
▶ Medical Interventions: Cardiac or neurological treatments depending on identified causes.
Treatment Options in Korea
Medical Evaluation:
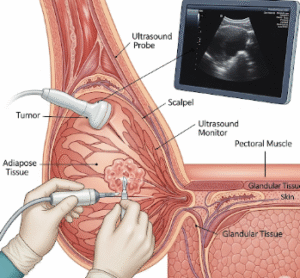
▶ Cardiology Consultation: ECG, echocardiography, Holter monitoring, or stress testing to detect cardiac causes.
▶ Neurology Assessment: EEG or brain imaging for seizure or neurological disorders.
▶ Blood Tests: Checking for anemia, electrolyte imbalances, or metabolic issues.
▶ Tilt Table Test: Evaluates autonomic nervous system response and orthostatic hypotension.
Advanced Therapies:
▶ Medication Management: Anti-arrhythmics, blood pressure regulators, or treatments for underlying neurological disorders.
▶ Surgical Interventions: Pacemaker implantation for heart block or structural cardiac abnormalities.
▶ Physical Therapy and Rehabilitation: Strengthening circulatory response, posture management, and fall prevention.
Rehabilitation & Support:
▶ Patient Education: Recognizing early warning signs, avoiding triggers, and implementing lifestyle modifications.
▶ Follow-Up Care: Regular monitoring of heart and neurological health.
▶ Specialist Clinics: Korean hospitals provide integrated care combining cardiology, neurology, and rehabilitation for comprehensive management.
Outcome: With timely assessment and treatment in Korea, most cases of blackouts can be managed safely, reducing the risk of injury, preventing recurrence, and improving overall quality of life.