Overview
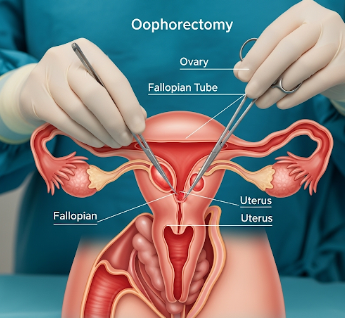
Oophorectomy is a surgical procedure to remove one or both ovaries. It is commonly performed to treat ovarian cysts, tumors, endometriosis, or as a preventive measure for those at high risk of ovarian or breast cancer. Oophorectomy can be unilateral (one ovary) or bilateral (both ovaries) depending on medical necessity.
In South Korea, oophorectomy is performed in highly specialized gynecological and oncology centers using laparoscopic, minimally invasive, or open surgical techniques, ensuring precision, safety, and optimal recovery.
What is Oophorectomy?
Oophorectomy involves surgically removing the ovary/ovaries to address disease or reduce cancer risk. Types include:
✔ Unilateral oophorectomy: Removal of one ovary, preserving fertility if possible.
➔ Bilateral oophorectomy: Removal of both ovaries, often for cancer prevention or treatment.
● Prophylactic oophorectomy: Preventive removal for patients with BRCA1/2 mutations or strong family history of ovarian/breast cancer.
★ Oophorectomy with hysterectomy: Removal of ovaries alongside the uterus in certain cases.
What are the Benefits?
Oophorectomy provides several medical benefits:
✔ Removes diseased or cancerous ovaries to prevent disease progression.
➔ Reduces risk of ovarian and breast cancer in high-risk individuals.
● Alleviates chronic pain from ovarian cysts, endometriosis, or pelvic pathology.
★ Prevents recurrence in patients with prior ovarian tumors.
➤ May be combined with other procedures for comprehensive gynecologic care.
Procedure Details
1) How should I prepare for Oophorectomy?
Preparation is essential for safe surgery:
✔ Medical evaluation: Blood tests, imaging (ultrasound, CT, MRI), and cancer markers.
➔ Medication review: Blood thinners or anticoagulants may need to be paused.
● Fasting: Typically 6–8 hours before surgery under general anesthesia.
★ Patient counseling: Discuss procedure type, risks, fertility implications, and hormone replacement therapy if needed.
➤ Lifestyle adjustments: Smoking cessation and maintaining hydration for optimal healing.
2) What happens during the procedure Oophorectomy?
Oophorectomy can be performed laparoscopically or via open surgery:
✔ Anesthesia: General anesthesia ensures comfort and safety.
➔ Incision: Small laparoscopic ports or larger abdominal incision (laparotomy).
● Ovary removal: Surgeon detaches ovary/ovaries from surrounding tissue and blood vessels.
★ Adjunct procedures: May include hysterectomy or lymph node sampling if indicated.
➤ Closure: Incisions sutured and sterile dressings applied; laparoscopic surgery involves minimal scarring.
✔ Duration: Usually 1–2 hours for laparoscopic, longer for open surgery or combined procedures.
Korean hospitals frequently use advanced laparoscopy and robotic-assisted surgery to enhance precision and reduce recovery time.
3) What happens after Oophorectomy?
Post-operative care focuses on healing and monitoring:
✔ Hospital stay: Typically 1–3 days for laparoscopic surgery; longer for open procedures.
➔ Pain management: Mild to moderate pain controlled with medications.
● Activity restrictions: Avoid heavy lifting, strenuous exercise, and sexual activity for 4–6 weeks.
★ Hormonal changes: Bilateral oophorectomy may induce surgical menopause; hormone replacement therapy may be recommended.
➤ Follow-up: Wound checks, imaging if needed, and hormone level monitoring.
Risks / Benefits
Possible Risks:
✔ Infection at surgical site
➔ Bleeding or hematoma
● Damage to surrounding organs (bladder, intestines, blood vessels)
★ Hormonal imbalance or early menopause (if both ovaries removed)
➤ Rare complications from anesthesia
Major Benefits:
✔ Eliminates diseased or cancerous ovaries
➔ Reduces risk of ovarian and breast cancer in high-risk patients
● Alleviates chronic pelvic pain
★ Can be combined with other gynecologic procedures for comprehensive treatment
➤ Minimally invasive techniques in Korea reduce recovery time and complications
Recovery and Outlook
✔ Initial recovery: 1–2 weeks for laparoscopic surgery; 4–6 weeks for open procedures.
➔ Activity: Gradual return to normal activities under guidance.
● Hormonal management: May require hormone replacement therapy if both ovaries are removed.
★ Long-term outlook: High success rate for disease treatment and cancer prevention; most patients regain normal daily function.
➤ Follow-up: Periodic check-ups, imaging, and lab tests ensure ongoing health.
When To Call the Doctor
Patients should contact their doctor if they notice:
✔ Severe or increasing pain
➔ Fever, redness, or discharge at incision site
● Persistent nausea or vomiting
★ Abnormal bleeding or swelling
➤ Symptoms of hormone imbalance (hot flashes, mood changes, fatigue)
Best Korea Option / Process
South Korea offers state-of-the-art oophorectomy treatment:
✔ Top hospitals: Asan Medical Center, Samsung Medical Center, Seoul National University Hospital.
➔ Advanced surgical techniques: Laparoscopic and robotic-assisted oophorectomy.
● Multidisciplinary care: Gynecologic surgeons, oncologists, anesthesiologists, and hormone specialists.
★ Comprehensive post-op support: Pain management, hormone therapy, counseling, and rehabilitation.
➤ Medical tourism support: Translation, travel coordination, and follow-up for international patients.
✅ Highlights:
✔ Oophorectomy removes one or both ovaries
➔ Treats ovarian disease, cancer, or reduces cancer risk
● Minimally invasive surgery ensures faster recovery
★ Risks include infection, bleeding, organ injury, and hormonal changes
➤ Korean hospitals provide advanced surgical care, post-op support, and high patient satisfaction