Overview
Mastectomy is a surgical procedure that removes all or part of the breast to treat or prevent breast cancer. It is a key option for women diagnosed with breast cancer or those at high risk due to genetic predisposition, family history, or other risk factors.
In Korea, mastectomy is performed by experienced breast surgeons using advanced surgical and reconstructive techniques, including minimally invasive approaches and immediate breast reconstruction options, ensuring effective cancer management while minimizing physical and emotional impact.
Highlights:
- ✅ Treats existing breast cancer or prevents high-risk breast cancer
- ✅ Can be combined with breast reconstruction
- ✅ Performed by expert surgeons in advanced medical centers
- ✅ Offers peace of mind for high-risk patients
What is Mastectomy — Breast Cancer Treatment or Prevention?
Mastectomy involves removing part or all of the breast tissue, including sometimes the nipple, areola, and nearby lymph nodes. It may be performed:
- Therapeutically: To remove cancerous tissue in patients diagnosed with breast cancer
- Prophylactically (Preventive): For patients at high risk of developing breast cancer (e.g., BRCA1 or BRCA2 gene mutations)
Types of mastectomy include:
- Total (Simple) mastectomy: Removes the entire breast without lymph nodes
- Modified radical mastectomy: Removes the breast and some lymph nodes
- Skin-sparing or nipple-sparing mastectomy: Preserves skin or nipple for reconstruction
- Bilateral prophylactic mastectomy: Removal of both breasts to reduce cancer risk
Important: The choice of mastectomy type depends on cancer stage, tumor size, genetics, and patient preference.
What are the benefits?
- Effective cancer treatment: Removes cancerous tissue and reduces recurrence risk
- Risk reduction for high-risk individuals: Significantly lowers chances of developing breast cancer
- Reconstruction options available: Immediate or delayed reconstruction improves cosmetic outcomes
- Peace of mind: Provides control for patients with genetic or family-related risk factors
Key benefits highlighted:
- ⚡ High effectiveness for cancer control or prevention
- ⚡ Can be combined with reconstruction for natural appearance
- ⚡ Minimizes anxiety for high-risk individuals
- ⚡ Tailored to patient’s medical and personal needs
Procedure Details
1) How should I prepare for Mastectomy?
- Preoperative evaluation: Mammograms, MRI, ultrasound, biopsy results, blood tests, and genetic counseling if preventive
- Medication review: Stop blood thinners or medications as instructed
- Fasting: Usually 6–8 hours before surgery
- Consent and education: Discuss type of mastectomy, reconstruction options, risks, and recovery
- Lifestyle preparation: Arrange for postoperative care and support
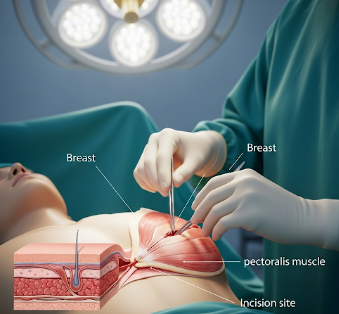
2) What happens during Mastectomy?
- Anesthesia: General anesthesia administered
- Incision and removal: Depending on type, breast tissue, nipple-areola complex, and possibly lymph nodes are removed
- Reconstruction (if chosen): Immediate reconstruction using implants or autologous tissue may be performed
- Closure: Incisions closed with sutures; drains may be placed to prevent fluid accumulation
Duration: Typically 2–4 hours depending on procedure complexity and reconstruction
3) What happens after Mastectomy?
- Recovery monitoring: Vital signs, drainage, and incision sites observed
- Pain management: Analgesics for moderate postoperative pain
- Activity: Gradual return to normal activities; avoid heavy lifting for several weeks
- Follow-up care: Monitor wound healing, drainage, and overall recovery
Highlights for post-procedure care:
- ⚡ Swelling, bruising, and mild discomfort are expected
- ⚡ Drains usually removed within 1–2 weeks
- ⚡ Avoid strenuous activity and heavy lifting for 4–6 weeks
- ⚡ Attend all follow-up visits for monitoring and reconstruction assessment
Risks / Benefits
Risks:
- Infection or bleeding
- Seroma (fluid accumulation)
- Numbness or altered sensation in chest or arm
- Scarring or asymmetry
- Lymphedema if lymph nodes are removed
- Anesthesia-related complications
Benefits:
- Effective treatment of breast cancer
- Reduces recurrence risk
- Preventive option for high-risk individuals
- Can be combined with reconstruction for improved appearance
Recovery and Outlook
- Hospital stay: Typically 1–3 days for simple mastectomy; 3–5 days if reconstruction performed
- Full recovery: 4–6 weeks for normal activities; 6–8 weeks before full physical activity
- Long-term outlook: Excellent for both treatment and preventive cases when combined with follow-up care
- Follow-up: Regular monitoring with oncology and reconstructive teams; continued imaging or preventive care as indicated
Tips for optimal recovery:
- ✅ Follow wound care instructions
- ✅ Wear compression garments if recommended
- ✅ Gradually resume daily activities as advised
- ✅ Attend all follow-up appointments for health monitoring and reconstruction evaluation
When To Call the Doctor
- Fever, chills, or signs of infection
- Excessive bleeding or fluid accumulation
- Severe or uncontrolled pain
- Unusual swelling in the chest or arm
- Any concerns about reconstruction or wound healing
Best Korea Option / Process
Korea provides advanced mastectomy care for both treatment and prevention:
- Top hospitals: Specialized breast cancer centers with expert surgeons
- Surgical expertise: Wide range of mastectomy types and reconstruction options
- Advanced imaging: Preoperative planning with mammography, MRI, and ultrasound
- Postoperative care: Pain management, wound monitoring, drainage care, and rehabilitation
- International patient support: Online consultations, appointment scheduling, and telemedicine follow-up
Step-by-step process in Korea:
- Preoperative consultation and imaging review
- Selection of mastectomy type and reconstruction plan
- Surgery performed by expert breast surgeons under general anesthesia
- Postoperative monitoring, pain management, and gradual activity resumption
- Follow-up visits to monitor healing, reconstructive results, and overall health