Overview
The Kasai Procedure, also known as hepatoportoenterostomy, is a surgical treatment primarily used for infants with biliary atresia, a condition where the bile ducts are blocked or absent. This procedure restores bile flow from the liver to the intestines, preventing liver damage and improving long-term liver function.
South Korea is recognized for expert pediatric surgeons, advanced neonatal care, and specialized post-operative monitoring, making it a leading destination for families seeking safe, effective, and life-saving biliary surgery for children.
What is the Kasai Procedure?
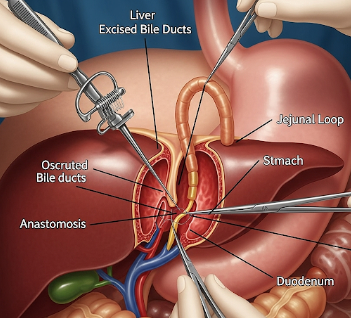
The Kasai Procedure involves:
- Removal of the blocked bile ducts outside the liver
- Reconstruction using a loop of the small intestine (usually jejunum) to create a new bile drainage pathway
- Restoration of bile flow to prevent cholestasis and liver fibrosis
Indications:
- Biliary atresia in newborns and infants
- Early-stage cholestatic liver disease caused by bile duct obstruction
- Failure of bile drainage leading to jaundice, poor growth, or liver injury
Goal:
- Prevent progression to cirrhosis and liver failure
- Delay or reduce the need for liver transplantation
- Support normal growth, digestion, and development in infants
What are the Benefits?
- Restores bile flow → Reduces jaundice and bilirubin accumulation
- Preserves liver function → Helps maintain growth and overall health
- Delays or avoids liver transplantation → Particularly effective if performed early
- Improves digestion and nutrient absorption → Supports healthy development
- High success rates in specialized centers → Improved long-term survival
- Expert care in Korea → Experienced pediatric hepatobiliary surgeons and neonatal support
Procedure Details
1) How should I prepare for the Kasai Procedure?
- Preoperative evaluation → Blood tests, liver function tests, ultrasound, and sometimes MRI or cholangiography
- Medical optimization → Treat infections, improve nutrition, and manage coexisting conditions
- Medication review → Adjust anticoagulants, antibiotics, or other medications
- Pre-procedure consultation → Discuss surgical steps, anesthesia, expected outcomes, and post-operative care
- Parental preparation → Understand procedure risks, post-op care, and potential need for liver transplantation
2) What happens during the procedure?
- Anesthesia → General anesthesia for complete sedation
- Patient positioning → Supine with careful neonatal support
- Surgical steps →
- Abdominal incision to access liver and bile ducts
- Removal of the damaged or blocked extrahepatic bile ducts
- Creation of a Rou-en-Y jejunal loop to connect the liver to the small intestine
- Ensuring bile drainage is established and secured
- Closure of abdominal incision with careful suturing
- Duration → Typically 2–4 hours depending on complexity and patient size
- Monitoring → Continuous vital signs, oxygenation, and neonatal monitoring
3) What happens after the procedure?
- Immediate post-operative care → ICU or high-dependency monitoring for infants
- Nutrition and feeding → Gradual introduction of oral or tube feeding; sometimes parenteral nutrition initially
- Medication → Antibiotics, ursodeoxycholic acid, and fat-soluble vitamin supplementation
- Activity restrictions → Infants remain in controlled environment; parents educated on handling
- Follow-up visits → Frequent monitoring of liver function, bilirubin levels, and growth parameters
Risks / Benefits
Risks
- ➤ Infection at surgical site or within abdomen
- ➤ Bleeding or bile leakage
- ➤ Anastomotic stricture or obstruction
- ➤ Liver damage despite surgery in some cases
- ➤ Need for liver transplantation if Kasai procedure fails
Benefits
- ➤ Restores bile flow and improves liver function
- ➤ Supports growth and development in infants
- ➤ Delays or reduces the need for liver transplantation
- ➤ Minimally invasive techniques in specialized centers
- ➤ High success rates with expert pediatric surgical care in Korea
Recovery and Outlook
- Immediate recovery → ICU care with monitoring for bile flow, infection, and nutrition
- Short-term follow-up → Blood tests, ultrasound, and bilirubin monitoring
- Long-term follow-up → Periodic liver function tests, growth assessment, and nutritional support
- Expected outcomes →
- Successful bile flow in 60–80% of infants if performed early
- Improved growth, digestion, and liver function
- Some patients may still require liver transplantation later in life
- Post-procedure care → Regular medical check-ups, vitamin supplementation, and monitoring for complications
- Support → Korean pediatric centers provide family education and multidisciplinary care
When To Call the Doctor
Contact your pediatric surgeon immediately if you notice:
- ⚠️ Persistent jaundice or dark urine
- ⚠️ Fever, vomiting, or signs of infection
- ⚠️ Abdominal swelling or tenderness
- ⚠️ Poor feeding or growth stagnation
- ⚠️ Any unusual bleeding or stool changes
Best Korea Option / Process
South Korea is a leading destination for the Kasai Procedure due to:
- Expert pediatric hepatobiliary surgeons
- State-of-the-art neonatal and pediatric surgical facilities
- Multidisciplinary care including hepatology, nutrition, and anesthesiology
- Comprehensive post-operative monitoring and family support
- International patient services → Consultation, translation, scheduling, and follow-up
Top Hospitals for Kasai Procedure in Korea:
- Asan Medical Center, Seoul – Advanced pediatric liver surgery and Kasai expertise
- Samsung Medical Center – Specialized pediatric hepatobiliary care
- Seoul National University Hospital (SNUH) – Multidisciplinary neonatal and pediatric surgery
- Yonsei Severance Hospital – Comprehensive liver and biliary care for infants
👉 For infants with biliary atresia or bile duct obstruction, Kasai Procedure in Korea offers life-saving surgery with expert care, high success rates, and comprehensive post-operative support.