As South Korea enters 2026, hospitals across the country are anticipating and preparing for several major policy changes and reforms. These adjustments reflect shifting demographics, evolving healthcare challenges, and political priorities. The policy shifts will influence hospital funding, staffing, patient care models, and regulatory oversight. Below are key reforms to watch and what they may mean for hospitals and patients.
1. Bigger Public Healthcare Budget, Focus on Regional Equity
The Ministry of Health and Welfare has proposed a 2026 budget of ₩137.64 trillion, marking a 9.7 % increase over the previous year. This increase is intended to expand essential medical services, strengthen public and regional healthcare infrastructure, and support training for medical professionals.
Hospitals in underserved or rural regions may gain more support to upgrade facilities, recruit staff, and expand capacity.
This budget expansion reflects a government push to reduce disparities between urban major hospitals and smaller regional ones.
➡ Hospitals outside top-tier cities may receive more subsidies, grants, or preferential investment in 2026.
➡ National cancer and cardiovascular disease management budgets are also rising, which may shift patient loads and funding allocations for hospital departments.
Reference: health ministry budget plans KBR
2. Reclassification of Major Hospitals (Tier-4 Designation)
The Presidential Committee on Healthcare Reform has floated plans to designate Korea’s five major hospitals (Seoul National University Hospital, Asan Medical Center, Severance, Samsung Medical Center, St. Mary’s) as “tier-4 hospitals” specializing in critical or severe care.
Under this scheme:
- These tier-4 hospitals would focus on trauma, rare diseases, critical care, and high-complexity cases.
- Routine or lower-acuity cases might be directed to smaller or regional hospitals, helping redistribute patient loads.
- The aim is to reduce overcrowding and improve specialization.
For hospitals, this may mean more pressure to specialize, upgrade equipment, and maintain cutting-edge capabilities.
Smaller hospitals might see increased demand for general or non-critical services.
Reference: plans to elevate major hospitals 조선일보
3. Increased Fees for Severe Illness Treatment
To incentivize care for high-complexity cases, the government plans to raise reimbursements for doctors and hospitals treating severe illnesses, intensive care, and critical surgeries.
- A 50 % fee hike is expected for ICU services and certain high-risk surgical procedures.
- Over three years, around ₩10 trillion will be allocated from health insurance funds for this purpose.
- The goal is to shift 70 % of case volume in major hospitals toward severe illnesses, up from ~50 % currently.
For hospitals, this provides financial incentive to maintain and expand critical care capacity, while potentially reducing reliance on non-severe or high-volume, low-margin services.
Reference: fee hikes for severe illness care Reuters
4. Medical Staff Quota Reform and Doctor Shortage
A core contested reform has been raising the quota of medical students by 2,000 per year starting 2025, meant to ease doctor shortages, especially in rural areas and underserved specialties.
- Due to protests from medical communities, the government has slowed the increase in 2025, but the full quota increase is still slated for 2026. AP News+1
- Hospitals will need to plan for a larger influx of trainees, residents, and interns.
- Some hospitals—especially teaching hospitals—may need to expand educational infrastructure (more training slots, supervisory staff, facilities).
- However, hospitals might also face pressure to absorb more trainees into specialties where shortages have been acute (e.g. pediatrics, obstetrics, emergency).
This reform touches on tension between supply of doctors, training quality, and hospital capacities.
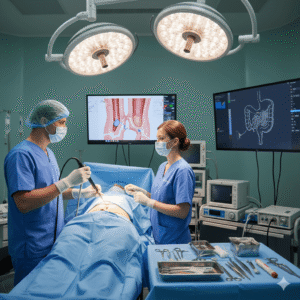
5. Emergency Care & ER Reform
Emergency rooms in Korea have long faced strain due to staffing shortages and overcrowding. The government acknowledges this crisis as a central driver for medical reform. The Korea Times+1
In 2026, hospitals may face stricter guidelines or restructuring mandates regarding ER operations:
- Hospitals may be required to ensure minimum staffing levels or shift coverage in emergency departments.
- Some emergency care may be routed to specialized or designated hospitals (e.g. the tier-4 hospitals above).
- Hospitals may see funding incentives or penalties tied to ER wait times, patient outcomes, or resource use.
For hospital administrators, this means rethinking resource allocation, cross-department support (e.g. internal medicine, intensive care), and possibly scaling back non-emergency workload during critical times.
6. Smart Hospitals and Digital Health Mandates
South Korea has actively promoted smart hospital development—hospitals equipped with advanced IT, AI-based systems, telemedicine, and patient-centered tech. Healthcare IT News
In 2026:
- Some hospitals may be required or pushed to meet digital health benchmarks (electronic records, AI diagnostics, integration, predictive analytics).
- Government programs may provide matching funds or subsidies for hospitals upgrading digital infrastructure.
- Hospitals that lag in “smart readiness” may face disadvantages in reimbursement or public reputation.
Thus, digital transformation becomes more of a necessity than optional modernization.
7. More Integrated Bio / Biotechnology Collaboration
With the establishment of the Presidential Bio Committee in 2025, policies are increasingly aligning biotechnology, clinical research, pharmaceuticals, and medical services under a cohesive strategy. Wikipedia
In 2026, hospitals that act as clinical research centers or that partner in biotech R&D may receive support or preferred status.
Expect more incentives for hospitals to host clinical trials, translational research, and biotech collaborations—especially in advanced therapeutics.
8. Efforts to Contain Healthcare Costs
Korea faces strong demographic pressures: a rapidly aging society and rising healthcare demand. Korea Economic Institute of America+1
To control spending, policies may push hospitals to:
- More aggressive cost efficiency (lean operations, resource optimization)
- Shift non-critical care away from high-cost hospitals
- Emphasize preventive, outpatient, home-based care over expensive inpatient or specialty services
- Adjust reimbursement rates, limit overuse of high-cost technologies
For hospitals, this will require balancing cost pressures with quality, patient satisfaction, and innovation.
9. Enhanced Regulation & Oversight
Policy changes will likely accompany stronger regulatory oversight in hospital operations:
- More frequent audits and performance evaluations tied to funding or reimbursement
- Stricter compliance requirements for safety, data management, quality control
- Requirements for transparency in outcomes, patient satisfaction, operational efficiency
- Potential penalties for underperformance or poor outcomes
Hospitals will need to bolster compliance departments, data systems, and governance to adapt.
🚑 What Hospitals and Clinics Should Do
➡ Strategic resource planning: Anticipate staffing changes, infrastructure needs, and departmental shifts (especially in emergency and critical care).
➡ Upgrade digital systems: Invest in EMRs, AI tools, telemedicine, and interoperability to stay competitive.
➡ Strengthen partnerships: Connect with biotech firms, research institutions, and government programs to access funding and new opportunities.
➡ Financial modeling: Project impacts of fee increases, reimbursement shifts, and sliding-volume policies to adjust service portfolios.
➡ Quality and compliance readiness: Be prepared for stricter performance oversight and data transparency requirements.
➡ Focus on specialization: For larger hospitals, leaning more into high-complexity care may be strategic under the new tiering scheme.
These policy changes reflect a deliberate shift in how Korea envisions its hospital sector: more equitable access, regional balance, cost discipline, technological integration, and global competitiveness. For hospital administrators, clinicians, and health system planners, 2026 will be a year of adaptation, investment, and potentially transformation.