Overview
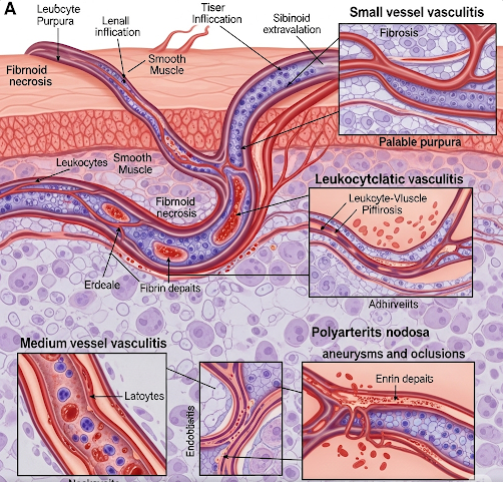
Vasculitis is an inflammation of the blood vessels, which can affect arteries, veins, or capillaries. The condition can cause blood vessel walls to thicken, weaken, narrow, or scar, reducing blood flow to vital organs and tissues. Vasculitis can occur as a short-term (acute) illness or a long-term (chronic) condition. It may be triggered by infections, autoimmune disorders, medications, or unknown causes. The severity ranges from mild to life-threatening, depending on the blood vessels and organs affected.
What is Vasculitis?
Vasculitis is not a single disease but a group of disorders involving inflammation of blood vessels. This inflammation can lead to vessel damage, impairing oxygen and nutrient delivery throughout the body. Types of vasculitis include giant cell arteritis, Takayasu arteritis, polyarteritis nodosa, granulomatosis with polyangiitis, and Kawasaki disease. Vasculitis can affect any part of the body and may involve multiple organs.
Symptoms
Symptoms vary depending on the type and location of affected vessels but may include:
- Fever and fatigue
- Muscle and joint pain
- Unexplained weight loss
- Skin rashes, red spots, or ulcers
- Numbness or weakness in limbs
- Headaches and vision problems (if brain arteries are involved)
- Abdominal pain or digestive issues (if gastrointestinal arteries are affected)
- Shortness of breath or chest pain (if heart or lung vessels are involved)
Causes
- Autoimmune response – The immune system mistakenly attacks blood vessels
- Infections – Hepatitis B, hepatitis C, and other viral or bacterial infections
- Medications – Certain drugs can trigger hypersensitivity reactions
- Genetic predisposition – Family history of autoimmune diseases
- Underlying diseases – Lupus, rheumatoid arthritis, or other connective tissue disorders
- Unknown causes – Many cases are idiopathic
Risk Factors
- Middle-aged or older adults (for certain types like giant cell arteritis)
- Family history of autoimmune diseases
- Chronic infections
- Certain genetic markers
- Existing autoimmune disorders
Complications
If left untreated, vasculitis can cause:
- Organ damage due to reduced blood flow
- Aneurysms (weakened, bulging vessel walls)
- Blood clots
- Vision loss (in giant cell arteritis)
- Kidney failure
- Permanent nerve damage
Prevention
There is no guaranteed prevention for vasculitis, but risk can be reduced by:
- Managing underlying autoimmune or infectious diseases
- Avoiding medications known to trigger vasculitis (when possible)
- Maintaining a healthy immune system with balanced diet and lifestyle
- Regular check-ups for early detection in high-risk individuals
Treatment Options in Korea
South Korea provides advanced, multidisciplinary treatment for vasculitis, focusing on controlling inflammation and preventing organ damage:
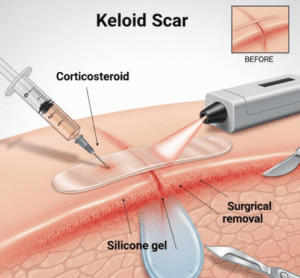
- Corticosteroids – Such as prednisone to quickly reduce inflammation
- Immunosuppressive drugs – Cyclophosphamide, azathioprine, or methotrexate for long-term control
- Biologic therapies – Rituximab or tocilizumab for resistant cases
- Plasmapheresis – Blood filtering to remove harmful antibodies in severe cases
- Antiviral therapy – For infection-related vasculitis (e.g., hepatitis B or C treatment)
- Organ-specific care – Specialized treatment for kidney, heart, lung, or nervous system complications
- Advanced diagnostics – Korean hospitals use PET scans, MRI, and angiography to monitor disease activity and treatment response