Overview
Uveitis is a group of inflammatory conditions affecting the uvea, the middle layer of the eye. It can cause redness, pain, blurred vision, and sensitivity to light, and may affect one or both eyes. If left untreated, uveitis can lead to serious complications, including vision loss or blindness. Prompt diagnosis and treatment are essential to preserve eyesight and manage underlying causes.
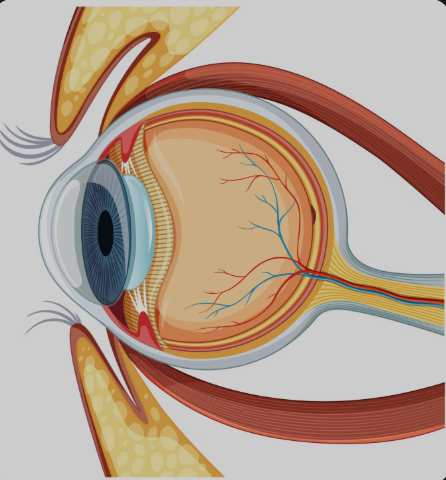
What is Uveitis
Uveitis is an inflammation of the uvea, which consists of the iris, ciliary body, and choroid—key structures responsible for nourishing the eye and controlling light entry. Uveitis can be classified based on the part of the eye affected:
- Anterior uveitis (iritis) – most common; affects the front of the eye
- Intermediate uveitis – affects the vitreous (gel-like fluid)
- Posterior uveitis – affects the retina and choroid
- Panuveitis – involves all layers of the uvea
Uveitis may result from autoimmune disorders, infections, trauma, or be idiopathic (of unknown origin).
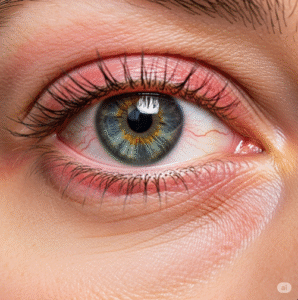
Symptoms
Symptoms can vary depending on the type and severity of the inflammation but commonly include:
- Eye redness and irritation
- Eye pain
- Blurred vision
- Light sensitivity (photophobia)
- Floaters (spots or shadows in vision)
- Decreased visual acuity
- Tearing or watery eyes
Symptoms may develop suddenly or gradually and often recur in chronic or relapsing cases.
Causes
Uveitis can have numerous causes, and identifying the underlying condition is crucial for effective treatment:
- Autoimmune diseases:
- Rheumatoid arthritis
- Ankylosing spondylitis
- Sarcoidosis
- Behçet’s disease
- Lupus
- Infections:
- Herpes simplex virus (HSV)
- Toxoplasmosis
- Tuberculosis
- Syphilis
- CMV (cytomegalovirus)
- Eye injury or trauma
- Post-surgical inflammation
- Idiopathic (unknown cause) – up to 50% of cases
Risk Factors
- Age between 20–60
- History of autoimmune or inflammatory diseases
- Recent eye trauma or surgery
- Infectious diseases (e.g., HIV, TB, herpes)
- Smoking
- Family history of inflammatory conditions
Complications
If untreated or poorly managed, uveitis can lead to serious, sometimes irreversible complications:
- Glaucoma
- Cataracts
- Macular edema
- Retinal damage or detachment
- Optic nerve damage
- Vision loss or permanent blindness
Early treatment greatly reduces the risk of these complications.
Prevention
While uveitis cannot always be prevented, certain steps can help reduce risk or detect it early:
- Manage chronic autoimmune or inflammatory conditions
- Treat infections promptly
- Protect the eyes from injury (e.g., with safety glasses)
- Avoid exposure to infectious agents
- Attend regular eye exams, especially with systemic disease
- Stop smoking, as it increases the risk of uveitis and its severity
Treatment Options in Korea
South Korea offers state-of-the-art diagnostic tools and expert ophthalmologic care for uveitis, ensuring both symptom relief and long-term eye health.
- Diagnosis:
- Comprehensive eye exam (slit-lamp, fundoscopy)
- Optical coherence tomography (OCT) to detect retinal swelling
- Blood tests and imaging to identify underlying causes
- Aqueous or vitreous sampling, if infection is suspected
- Treatment:
- Corticosteroid eye drops (for anterior uveitis)
- Oral or injected corticosteroids for more severe or posterior cases
- Immunosuppressive therapy for autoimmune-related uveitis
- Antiviral, antibacterial, or antifungal medications for infectious causes
- Surgery (e.g., vitrectomy) in advanced or refractory cases
- Follow-up care:
- Regular eye pressure monitoring
- Long-term care plans for chronic or recurrent uveitis
- Coordination with rheumatologists or infectious disease specialists, as needed
Korean eye hospitals offer integrated care, advanced imaging, and subspecialist expertise, helping patients recover vision and control inflammation effectively.