Overview
Uterine Cancer, most commonly known as Endometrial Cancer, is a type of cancer that begins in the lining of the uterus (endometrium). It is one of the most prevalent gynecological cancers, particularly affecting postmenopausal women. When diagnosed early, endometrial cancer is often curable, but delayed detection can lead to spread beyond the uterus. Awareness of risk factors and symptoms is vital for timely diagnosis and effective treatment.
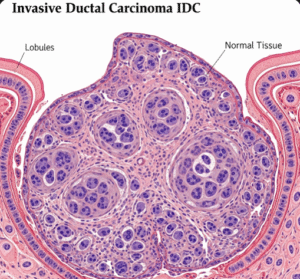
What is Uterine Cancer (Endometrial Cancer)
Uterine Cancer (Endometrial Cancer) is a malignant growth of cells in the endometrial lining of the uterus. The majority of uterine cancers are endometrioid adenocarcinomas, arising from glandular cells. It typically occurs after menopause but can also affect younger women, especially those with hormonal imbalances. Less commonly, uterine sarcomas can arise from the muscle or connective tissue of the uterus. The cancer is often detected early due to abnormal uterine bleeding.
Symptoms
Common symptoms include:
- Abnormal uterine bleeding (especially postmenopausal bleeding)
- Heavy or irregular periods (in premenopausal women)
- Pelvic pain or pressure
- Unusual vaginal discharge (watery or blood-tinged)
- Pain during intercourse
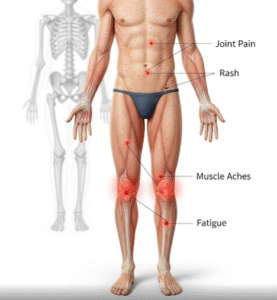
- Unintentional weight loss (in advanced cases)
- Fatigue or anemia (due to chronic blood loss)
Causes
Endometrial cancer develops due to uncontrolled cell growth in the uterine lining, usually driven by excess estrogen exposure without the balancing effect of progesterone. This hormonal imbalance can cause endometrial thickening and cellular abnormalities that may progress to cancer.
Risk Factors
- Postmenopausal status
- Obesity (increased estrogen from fat tissue)
- Polycystic ovary syndrome (PCOS)
- Estrogen-only hormone replacement therapy
- Early menstruation or late menopause
- Nulliparity (never having given birth)
- Diabetes
- Tamoxifen use (for breast cancer treatment)
- Lynch syndrome (hereditary nonpolyposis colorectal cancer)
- Family history of uterine or colon cancer
Complications
If not treated promptly, uterine cancer may lead to:
- Spread to nearby structures (cervix, fallopian tubes, ovaries)
- Metastasis to distant organs (lungs, liver, bones)
- Recurrent cancer after treatment
- Infertility (if diagnosed before completing childbearing)
- Surgical and treatment-related complications
- Psychological distress or hormonal imbalance after hysterectomy
Prevention
While not all cases are preventable, risk can be reduced by:
- Maintaining a healthy weight and active lifestyle
- Managing PCOS and diabetes
- **Using combined (estrogen + progesterone) hormone therapy if needed
- Monitoring for abnormal bleeding, especially after menopause
- Regular gynecological checkups
- Genetic counseling if family history suggests Lynch syndrome
- Considering use of oral contraceptives, which may reduce risk
Treatment Options in Korea
South Korea offers state-of-the-art diagnostics and personalized treatment strategies for uterine (endometrial) cancer, with a strong emphasis on early detection and fertility-sparing options when possible.
- Diagnosis:
- Pelvic ultrasound or transvaginal sonography
- Endometrial biopsy to examine tissue samples
- Hysteroscopy for direct visualization
- MRI or CT scans to assess spread
- Treatment (depending on cancer stage and patient’s fertility goals): Early-stage:
- Total hysterectomy (removal of uterus ± fallopian tubes and ovaries)
- Lymph node assessment
- Minimally invasive laparoscopic or robotic surgery
- Radiation therapy (external beam or internal brachytherapy)
- Hormone therapy (e.g., progestins) in hormone-receptor-positive cases
- Chemotherapy (e.g., carboplatin, paclitaxel)
- Targeted therapy and immunotherapy for recurrent/metastatic cases
- Fertility-preserving options (for early-stage, low-grade cases in young women):
- High-dose progestin therapy
- Regular endometrial surveillance
Korean hospitals provide multidisciplinary oncology care, combining gynecologic oncologists, radiologists, pathologists, and fertility specialists to ensure optimal outcomes.