Overview
Uterine Atony is a serious obstetric condition in which the uterus fails to contract effectively after childbirth, leading to severe postpartum hemorrhage (PPH). It is the most common cause of primary PPH, and if not promptly managed, it can result in significant blood loss, shock, and even maternal death. Immediate medical intervention is critical for stabilization and recovery.
What is Uterine Atony
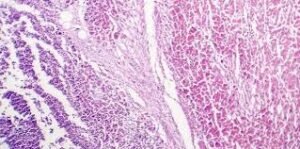
Uterine Atony refers to the inability of the uterine muscles to contract adequately after the delivery of the baby and placenta. Normally, uterine contractions compress the blood vessels at the placental site to prevent excessive bleeding. In uterine atony, this mechanism fails, leading to ongoing hemorrhage. It is a major obstetric emergency and requires fast diagnosis and aggressive treatment to preserve maternal health.
Symptoms
The hallmark symptom of uterine atony is heavy, uncontrolled bleeding after childbirth. Additional signs include:
- Excessive vaginal bleeding immediately after delivery
- Soft, boggy, or enlarged uterus on abdominal exam
- Low blood pressure (hypotension)
- Rapid heart rate (tachycardia)
- Pale or clammy skin
- Dizziness or fainting
- Signs of hypovolemic shock in severe cases
Causes
Uterine atony occurs due to failure of uterine muscle fibers (myometrium) to contract properly. Common causes include:
- Overdistended uterus (e.g., from multiple gestation, polyhydramnios, or a large baby)
- Prolonged or rapid labor
- Excessive use of oxytocin during labor
- High parity (many previous births)
- Infection or chorioamnionitis
- Retained placental fragments
- Use of certain anesthetics (e.g., halogenated agents)
- Manual removal of the placenta
Risk Factors
- Multiple pregnancies (twins or more)
- Macrosomia (baby > 4,000 grams)
- Prolonged labor or induced labor
- History of uterine atony or PPH
- Placenta previa or abruptio placentae
- General anesthesia use
- High maternal age
- Uterine abnormalities (e.g., fibroids)
Complications
If not promptly treated, uterine atony can lead to:
- Massive postpartum hemorrhage
- Hypovolemic shock
- Disseminated intravascular coagulation (DIC)
- Organ failure (kidneys, liver)
- Need for blood transfusions
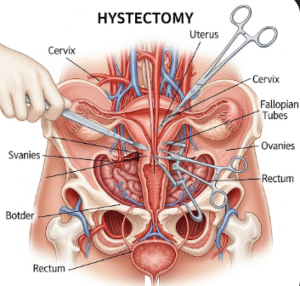
- Hysterectomy (removal of uterus)
- Maternal mortality
Prevention
While not all cases are preventable, risk reduction strategies include:
- Identifying high-risk patients before delivery
- Active management of the third stage of labor (e.g., administering oxytocin after delivery)
- Close monitoring during and after delivery
- Controlled delivery of the placenta
- Minimizing uterine overdistension (e.g., early detection of polyhydramnios or macrosomia)
- Early intervention at signs of excessive bleeding
Treatment Options in Korea
South Korea offers advanced, protocol-driven emergency obstetric care for uterine atony, ensuring timely management and reduced maternal risk:
- Initial interventions:
- Uterine massage to stimulate contractions
- Intravenous uterotonic medications (e.g., oxytocin, misoprostol, carboprost, ergometrine)
- Fluid resuscitation and blood transfusion, if necessary
- Further interventions:
- Manual removal of retained placental tissue
- Bakri balloon tamponade or uterine packing to apply pressure internally
- Surgical interventions:
- Uterine artery ligation
- Compression sutures (e.g., B-Lynch suture)
- Emergency hysterectomy if bleeding is uncontrollable
- Supportive care:
- ICU monitoring for severe cases
- Psychological support for affected mothers
- Postpartum follow-up to monitor recovery and anemia
Korean maternity hospitals follow evidence-based obstetric emergency protocols, using rapid response systems and experienced perinatal teams to manage uterine atony effectively and preserve fertility when possible.