Overview
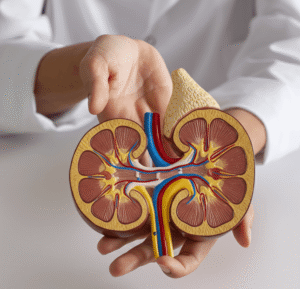
Urticarial Vasculitis is a rare form of vasculitis characterized by persistent, hive-like skin lesions that result from inflammation of the small blood vessels. Unlike typical urticaria (hives), the lesions in urticarial vasculitis are painful or burning, last longer than 24 hours, and may leave residual marks or bruising. The condition can be limited to the skin or may involve internal organs such as the kidneys, lungs, and joints.
What is Urticarial Vasculitis
Urticarial Vasculitis is an inflammatory disorder of the small blood vessels (leukocytoclastic vasculitis) that presents with chronic urticaria-like lesions. These lesions are caused by immune complex deposition in the blood vessels of the skin, leading to vascular inflammation. It can be divided into two types: normocomplementemic urticarial vasculitis (NUV) and hypocomplementemic urticarial vasculitis (HUV), the latter of which is more likely to be systemic and severe.
Symptoms
- Red or purplish hives that last longer than 24 hours
- Painful or burning sensation (rather than itching)
- Post-inflammatory hyperpigmentation or bruising
- Swelling (angioedema), especially of the lips and face
- Fever, fatigue, or malaise (especially in systemic cases)
- Joint pain or swelling (arthralgia)
- Abdominal pain
- Shortness of breath or cough (if lungs are affected)
- Kidney involvement (proteinuria or hematuria) in severe cases
Causes
The exact cause of urticarial vasculitis is unknown, but it is believed to be immune-mediated. Potential triggers or associations include:
- Autoimmune diseases (e.g., systemic lupus erythematosus, Sjögren’s syndrome)
- Chronic infections (e.g., hepatitis B/C, Epstein-Barr virus)
- Drug reactions (e.g., NSAIDs, antibiotics, ACE inhibitors)
- Malignancies (e.g., lymphomas)
- Serum sickness-like reactions
- Idiopathic (no identifiable cause)
Risk Factors
- Female gender (more commonly affected)
- Age 30–60 (most typical onset age)
- History of autoimmune conditions
- Long-term use of certain medications
- Chronic viral infections
- Family history of vasculitis or connective tissue disorders
Complications
Without proper diagnosis and treatment, urticarial vasculitis can lead to:
- Permanent skin discoloration or scarring
- Chronic pain and discomfort
- Organ involvement (lungs, kidneys, joints)
- Hypocomplementemia
- Glomerulonephritis
- Pulmonary complications (e.g., obstructive airway disease)
- Decreased quality of life due to relapsing symptoms
Prevention
There is no specific prevention for urticarial vasculitis, but the following may reduce risk or help manage symptoms:
- Avoid known triggers, such as certain drugs or allergens
- Monitor and manage autoimmune conditions
- Routine follow-up for people with connective tissue disorders
- Early evaluation of persistent urticaria lasting >24 hours
- Use sun protection, as UV exposure may trigger flares in some patients
- Control infections promptly to avoid immune system overactivity
Treatment Options in Korea
South Korea provides comprehensive care for urticarial vasculitis through a multidisciplinary approach, involving dermatologists, rheumatologists, and immunologists.
- Diagnosis:
- Skin biopsy to confirm leukocytoclastic vasculitis
- Blood tests: complement levels (C3, C4), ANA, ESR, CRP
- Urine tests: to assess kidney function
- Chest X-ray or CT scan for systemic evaluation
- Treatment:
- Antihistamines: for mild cases
- Corticosteroids: systemic steroids (e.g., prednisone) for moderate to severe inflammation
- Immunosuppressants: such as azathioprine, methotrexate, or mycophenolate mofetil for systemic involvement
- Hydroxychloroquine: often used in autoimmune-related cases
- Biologics: rituximab or omalizumab in resistant cases
- Plasmapheresis or IVIG: in severe, life-threatening systemic vasculitis
Korean hospitals utilize advanced diagnostic labs and individualized therapy plans, ensuring excellent monitoring and long-term control of the disease with minimal side effects.