Overview
Urothelial Carcinoma, also known as Transitional Cell Carcinoma, is the most common type of bladder cancer, though it can also affect the ureters, renal pelvis, and urethra. This cancer originates in the urothelium, the inner lining of the urinary tract. It can range from low-grade, non-invasive tumors to aggressive, muscle-invasive disease. Early detection and proper treatment are critical to improving outcomes and preserving urinary function.
What is Urothelial Carcinoma (Transitional Carcinoma)
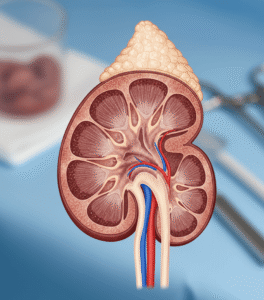
Urothelial Carcinoma (Transitional Carcinoma) is a malignant tumor arising from the urothelial cells lining the urinary tract, particularly the bladder, but also the ureters, renal pelvis, and urethra. It is the most prevalent type of bladder cancer, accounting for approximately 90% of all bladder tumors. The term “transitional” refers to the flexibility of urothelial cells, which can stretch and contract. These tumors are classified as non-muscle-invasive or muscle-invasive, with treatment and prognosis varying accordingly.
Symptoms
Symptoms may be mild in early stages but become more noticeable as the cancer progresses:
- Blood in urine (hematuria) – often painless and the most common early symptom
- Frequent urination
- Painful urination (dysuria)
- Urgency to urinate
- Pelvic or lower back pain (especially in advanced cases)
- Fatigue or unexplained weight loss
- Swelling in the legs (if tumor obstructs lymph drainage)
Causes
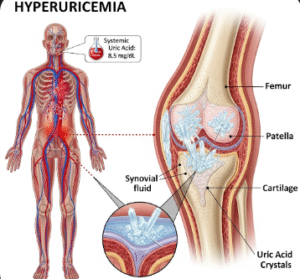
Urothelial carcinoma develops due to genetic mutations and cellular changes triggered by environmental and lifestyle factors:
- Tobacco smoking – the strongest risk factor
- Occupational exposure to chemicals (e.g., in dye, rubber, leather, and chemical industries)
- Chronic bladder irritation (from long-term catheter use, infections, or stones)
- Exposure to radiation therapy targeting the pelvic area
- Certain chemotherapy drugs (e.g., cyclophosphamide)
- Genetic predisposition or family history of bladder cancer
Risk Factors
- Smoking (responsible for nearly half of all cases)
- Age > 55 years
- Male gender
- Occupational chemical exposure
- Chronic urinary tract infections or bladder inflammation
- Personal or family history of bladder cancer
- Use of certain herbal medications containing aristolochic acid
- Previous pelvic radiation therapy
Complications
If left untreated or diagnosed late, urothelial carcinoma can lead to:
- Invasion of surrounding muscle and tissues
- Metastasis to lymph nodes, lungs, liver, or bones
- Urinary obstruction
- Hematuria-related anemia
- Bladder removal (cystectomy) and loss of bladder function
- Recurrence, even after treatment
- Impaired kidney function if upper urinary tract is involved
Prevention
While not all cases are preventable, the following steps can reduce risk:
- Stop smoking – the most effective prevention strategy
- Avoid occupational exposure to industrial chemicals with protective gear
- Drink plenty of fluids to flush the urinary tract
- Practice regular urination to avoid bladder irritation
- Monitor and manage chronic bladder conditions
- Regular check-ups for those with a family history or prior diagnosis
- Avoid unregulated herbal products known to be nephrotoxic or carcinogenic
Treatment Options in Korea
South Korea offers world-class cancer care with cutting-edge diagnostic tools, targeted therapies, and multidisciplinary management for urothelial carcinoma.
- Diagnosis:
- Urinalysis and urine cytology to detect cancer cells
- Cystoscopy – direct visual inspection and biopsy of bladder lining
- CT urogram or MRI to assess tumor extent and metastasis
- Transurethral resection of bladder tumor (TURBT) for staging
- Treatment (based on stage and grade): For non-muscle-invasive bladder cancer (NMIBC):
- TURBT followed by intravesical therapy (e.g., BCG or mitomycin C)
- Close surveillance with cystoscopy and urine testing
- Radical cystectomy (bladder removal) with urinary diversion
- Neoadjuvant or adjuvant chemotherapy
- Bladder-preserving trimodal therapy (TURBT + chemotherapy + radiation)
- Systemic chemotherapy
- Immunotherapy (e.g., checkpoint inhibitors)
- Targeted therapies for tumors with specific genetic mutations
- Palliative care and pain management, if needed
South Korean cancer centers are equipped with robot-assisted surgery, personalized oncology programs, and clinical trials, offering patients advanced treatment with internationally recognized outcomes.