Overview
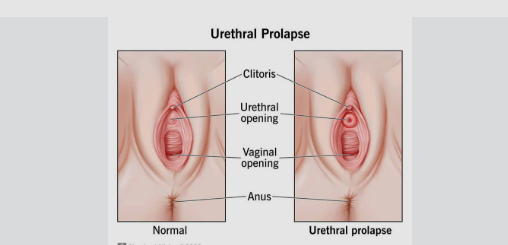
Urethral Prolapse is a condition in which the inner lining of the urethra protrudes through the external urethral opening. It most commonly affects prepubertal girls and postmenopausal women due to weakened pelvic tissues and low estrogen levels. Though usually benign, it can cause discomfort, bleeding, and urinary issues. Prompt diagnosis and treatment are important to relieve symptoms and prevent complications.
What is Urethral Prolapse
Urethral Prolapse is a circular protrusion of the distal urethral mucosa through the external urethral meatus. This condition occurs when the inner urethral lining loses its support and slips outward, forming a donut-shaped mass around the urethral opening. It is most commonly seen in young girls (ages 4–10) and postmenopausal women, due to hormonal changes, particularly low estrogen levels. Though rare, it may also affect women of reproductive age and very rarely men.
Symptoms
- A round, red or pink bulging mass at the urethral opening
- Vaginal bleeding or spotting (often mistaken for menstruation in young girls)
- Pain or burning during urination (dysuria)
- Urinary frequency or urgency
- Difficulty urinating or weak stream
- Irritation, itching, or discomfort in the genital area
- Urinary incontinence (in some cases)
- Asymptomatic in mild cases, discovered during routine exam
Causes
Urethral prolapse results from a combination of mechanical stress and hormonal deficiency that weakens the support structures of the urethra:
- Estrogen deficiency, especially in postmenopausal women or prepubertal girls
- Increased intra-abdominal pressure, due to chronic coughing, obesity, or straining
- Childbirth trauma or pelvic surgery
- Urinary tract infections or chronic inflammation
- Pelvic floor muscle weakness
- Connective tissue disorders (rare)
Risk Factors
- Prepubertal girls
- Postmenopausal women
- African descent (higher incidence in certain populations)
- Obesity
- Chronic constipation or coughing
- Pelvic organ prolapse
- Estrogen deficiency or hormonal changes
- History of pelvic surgery or trauma
Complications
- Ulceration or necrosis of the prolapsed tissue
- Recurrent urinary tract infections
- Hematuria (blood in the urine)
- Urinary retention or incontinence
- Painful urination or sexual discomfort
- Emotional distress, particularly in children
- Misdiagnosis (often confused with abuse, tumors, or other conditions)
Prevention
Although not always preventable, certain steps can help reduce the risk or recurrence of urethral prolapse:
- Maintain good perineal hygiene
- Use topical estrogen cream in at-risk postmenopausal women (as advised)
- Manage constipation and avoid straining during bowel movements
- Treat chronic cough or respiratory issues to minimize abdominal pressure
- Pelvic floor strengthening exercises (e.g., Kegels)
- Early treatment of urinary tract infections or genital irritation
Treatment Options in Korea
South Korea offers both conservative and surgical treatment options for urethral prolapse, ensuring comfort and recovery for patients of all ages:
- Topical estrogen cream: First-line treatment to reduce inflammation and restore tissue tone
- Warm sitz baths: To reduce swelling and promote healing
- Topical antibiotic or steroid creams: If signs of infection or inflammation are present
- Pain management: Mild analgesics or anti-inflammatory medications
- Manual reduction: Gently repositioning the prolapsed tissue (in some cases)
- Surgical excision:
- Indicated for persistent, large, or ulcerated prolapse
- Minimally invasive procedures with good cosmetic and functional outcomes
- Postoperative care: Includes estrogen therapy, hygiene education, and regular follow-up
Korean healthcare facilities offer pediatric and gynecologic specialists experienced in diagnosing and managing urethral prolapse with precision and sensitivity, especially in pediatric patients and elderly women.