Overview
Urea Cycle Disorder (UCD) is a rare inherited metabolic condition in which the body is unable to properly eliminate ammonia—a toxic waste product produced during protein metabolism. Ammonia accumulates in the blood (hyperammonemia), leading to potentially life-threatening symptoms, especially in newborns and young children. Early diagnosis, dietary management, and medical intervention are critical to prevent neurological damage and other complications.
What is Urea Cycle Disorder
Urea Cycle Disorder (UCD) is a group of inherited genetic conditions that affect the body’s ability to remove excess nitrogen in the form of urea. The urea cycle normally converts ammonia—produced when the body breaks down protein—into urea, which is then excreted in the urine. In UCD, a deficiency in one of the enzymes involved in this cycle causes ammonia to build up in the blood. High levels of ammonia are toxic, particularly to the brain, and can result in seizures, coma, and death if not promptly treated.
Symptoms
Symptoms vary depending on the age of onset and severity of the enzyme deficiency:
In newborns (within first few days of life):
- Poor feeding
- Vomiting
- Lethargy or sleepiness
- Irritability
- Breathing difficulties
- Seizures
- Coma
In children and adults:
- Recurrent vomiting
- Confusion or behavioral changes
- Headaches
- Lethargy or fatigue
- Protein intolerance
- Delayed growth or developmental issues
- Psychiatric symptoms (e.g., hallucinations, mood changes)
Causes
UCD is caused by mutations in any of the genes responsible for producing enzymes that function in the urea cycle. These include:
- CPS1 (Carbamoyl phosphate synthetase I deficiency)
- OTC (Ornithine transcarbamylase deficiency – most common and X-linked)
- ASS1 (Citrullinemia type I)
- ASL (Argininosuccinic acid lyase deficiency)
- ARG1 (Arginase deficiency)
- NAGS (N-acetylglutamate synthase deficiency)
These genetic defects are inherited in an autosomal recessive or X-linked pattern, depending on the specific type.
Risk Factors
- Family history of UCD or unexplained neonatal deaths
- Consanguineous (related) parents, increasing the risk of recessive inheritance
- Carrier mother of OTC deficiency, especially in male offspring
- Protein-rich diet or stressors (in adults with mild or late-onset UCD)
- Infections, surgeries, or medications that increase protein breakdown in the body
Complications
- Hyperammonemic coma, leading to brain damage or death
- Permanent neurological impairment, such as intellectual disability or developmental delays
- Liver dysfunction or failure
- Behavioral and psychiatric disorders
- Failure to thrive in infants and children
- Life-threatening crises, especially if untreated during infections or metabolic stress
- Recurrent hospitalizations due to metabolic instability
Prevention
Although UCD cannot be prevented due to its genetic origin, the following measures can help minimize its impact:
- Newborn screening (available in some countries for early detection)
- Prenatal genetic testing and counseling for at-risk families
- Avoid high-protein diets in diagnosed individuals
- Immediate medical care for infections or fever in known UCD patients
- Regular monitoring of ammonia levels and liver function
- Educate caregivers and schools about the signs of hyperammonemia
Treatment Options in Korea
South Korea offers advanced diagnostic and treatment services for rare metabolic disorders like UCD, delivered through specialized centers for pediatric and genetic diseases.
- Low-protein, high-calorie diet: Tailored by clinical nutritionists to reduce ammonia production
- Essential amino acid supplements: To support growth and protein needs
- Nitrogen-scavenging medications: Such as sodium benzoate and sodium phenylbutyrate to help eliminate excess nitrogen
- Arginine or citrulline supplements: Depending on the enzyme deficiency
- Ammonia level monitoring: Regular blood tests and emergency response plans
- Emergency treatment for hyperammonemic crises:
- Intravenous medications
- Dialysis to quickly remove ammonia
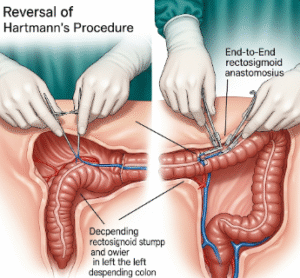
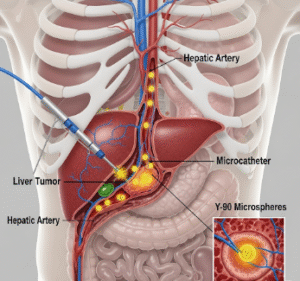
- Liver transplantation: Considered in severe or life-threatening cases for a long-term cure
- Genetic counseling: Offered to families with confirmed mutations or a history of UCD
Korea’s multidisciplinary approach ensures comprehensive care—from diagnosis and dietary planning to crisis management and long-term outcomes—for individuals with UCD.